WHO, 450 Million Facing Mental Health Disorders
World Health Organization 450 million people mental health disorders: A staggering 450 million people globally struggle with mental health disorders, a figure highlighting the urgent need for increased awareness and improved access to care. This represents a significant portion of the world’s population, impacting individuals across diverse socioeconomic backgrounds, ages, and geographical locations. The World Health Organization (WHO) plays a crucial role in addressing this global crisis, spearheading initiatives to improve mental healthcare access, raise awareness, and advocate for policy changes.
Understanding the scope of this challenge, the barriers to care, and effective interventions is critical to improving the lives of millions.
The distribution of these disorders is far from uniform. Factors like poverty, societal stigma, and limited access to healthcare disproportionately affect certain populations. This disparity necessitates targeted interventions tailored to specific communities and their unique needs. The following sections will explore the WHO’s efforts, the challenges faced by individuals seeking help, and the promising approaches to better mental health outcomes worldwide.
The WHO’s Role in Global Mental Health
The World Health Organization (WHO) plays a pivotal role in addressing the global mental health crisis. Its multifaceted approach encompasses advocacy, research, policy development, and the provision of technical support to countries worldwide. This commitment stems from the recognition that mental health is an integral component of overall well-being and essential for achieving sustainable development goals.
WHO Initiatives and Strategies
The WHO employs a range of strategies to improve global mental health. These include promoting the integration of mental healthcare into primary care systems, strengthening mental health workforce capacity, and advocating for policies that reduce stigma and discrimination. The organization also develops and disseminates evidence-based guidelines for the prevention and treatment of mental disorders.
Examples of WHO Programs
Several WHO programs directly address mental healthcare access. The Mental Health Gap Action Programme (mhGAP) provides guidance and tools for primary healthcare workers to identify and manage common mental disorders in resource-limited settings. The WHO’s work on suicide prevention focuses on raising awareness, strengthening community support systems, and restricting access to means of self-harm.
- mhGAP: Trains healthcare workers to identify and treat common mental disorders.
- Suicide Prevention: Promotes awareness campaigns and community support networks.
- Mental Health Action Plan 2013-2020: Set targets and strategies for improving mental health globally.
WHO’s Awareness Campaigns
The WHO actively campaigns to raise awareness about mental health issues. These campaigns utilize various media channels to challenge stigma, promote help-seeking behavior, and provide information on available resources. Successful campaigns often involve partnerships with governments, NGOs, and celebrities to maximize their reach and impact. For example, the WHO’s “Make Mental Health & Well-being for All a Global Priority” campaign emphasizes the importance of integrating mental health into all aspects of society.
The Scope of 450 Million People with Mental Health Disorders
The staggering figure of 450 million people living with mental health disorders represents a significant global health challenge. This population is diverse, encompassing individuals across all geographical locations, age groups, and socioeconomic strata. Understanding the distribution and characteristics of this population is crucial for developing effective interventions.
Global Distribution and Demographics
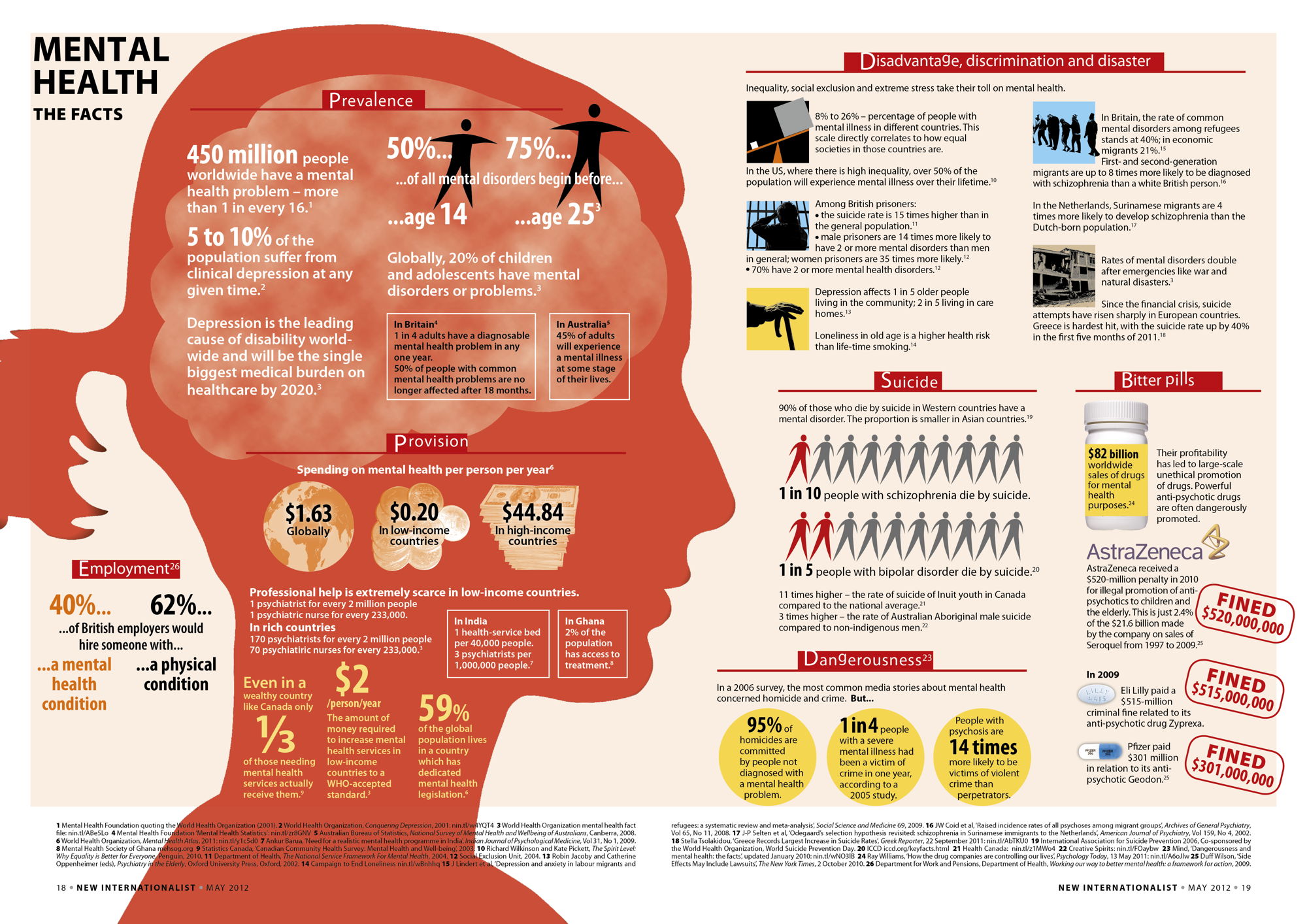
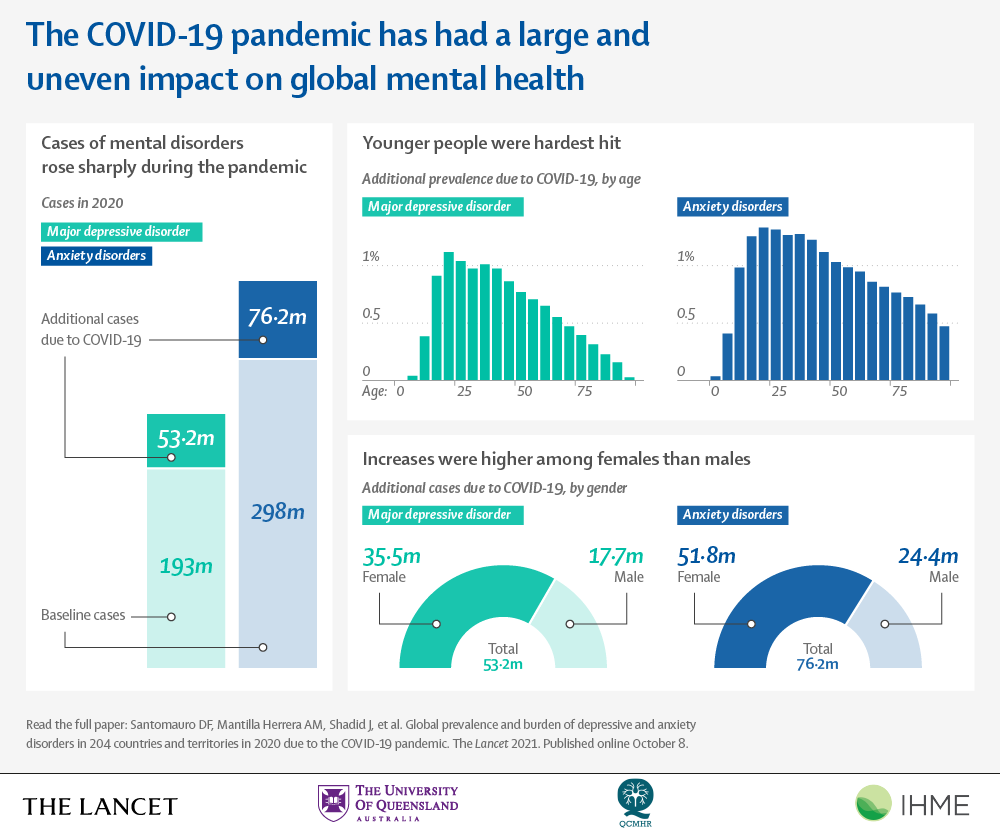
Mental health disorders are prevalent worldwide, though their distribution isn’t uniform. Low- and middle-income countries often face greater challenges in accessing mental healthcare due to limited resources and infrastructure. Age also plays a role, with certain disorders more common in specific age groups. For instance, depression and anxiety are prevalent among young adults, while dementia affects older populations.
Socioeconomic factors, including poverty and inequality, are strongly linked to increased risk and poorer outcomes.
Types and Severity of Mental Disorders
The 450 million individuals represent a broad range of mental health conditions. Depression and anxiety disorders are among the most common, followed by substance use disorders and schizophrenia. The severity of these disorders varies significantly, ranging from mild to severe, impacting individuals’ daily lives and functioning to varying degrees.
- Depression and anxiety disorders: Highly prevalent across various demographics.
- Substance use disorders: Often co-occur with other mental health conditions.
- Schizophrenia: A serious mental illness requiring specialized care.
Disproportionate Burden on Specific Groups
Certain demographic groups experience a disproportionately high burden of mental illness. Women, for instance, are more likely to experience anxiety and depression than men. Marginalized communities, including those facing poverty, discrimination, or conflict, also face heightened vulnerability. Children and adolescents are a particularly vulnerable group, with mental health conditions often going undiagnosed and untreated.
Barriers to Accessing Mental Healthcare
Numerous barriers impede access to mental healthcare, hindering timely diagnosis and treatment. These obstacles are complex and multifaceted, stemming from both systemic issues and individual-level factors.
Systemic and Individual Barriers, World health organization 450 million people mental health disorders
Systemic barriers include a lack of trained professionals, inadequate funding for mental health services, and limited access to medication. Stigma and discrimination, both at the societal and individual levels, represent major barriers to help-seeking behavior. Fear of judgment, social isolation, and concerns about confidentiality can prevent individuals from seeking help.
High-Income vs. Low-Income Country Challenges
While high-income countries face challenges such as long waiting lists and high costs of treatment, low-income countries grapple with a far greater scarcity of resources. The shortage of trained mental health professionals, limited access to medication, and the lack of integrated mental health services into primary care systems are particularly acute in low-income countries.
Impact of Stigma and Discrimination
Stigma surrounding mental illness is a powerful deterrent to seeking help. Individuals may fear being judged, discriminated against, or losing their jobs or relationships. This stigma can lead to delayed or forgone treatment, resulting in poorer outcomes and increased suffering.
Effective Mental Health Interventions
Evidence-based interventions are crucial for addressing the global mental health crisis. These interventions should be tailored to specific contexts, considering resource availability and cultural factors.
Interventions in Resource-Limited Settings
In resource-limited settings, cost-effective and scalable interventions are paramount. These include psychological therapies such as cognitive behavioral therapy (CBT) and interpersonal therapy (IPT), which can be delivered by trained lay providers. Pharmacological interventions, where available, can also play a vital role.
Role of Technology in Mental Healthcare
Technology offers significant potential for improving access to and delivery of mental healthcare services. Telehealth platforms, mobile apps, and online support groups can overcome geographical barriers and increase access to care, particularly in remote areas. Artificial intelligence (AI) is also being explored to improve diagnosis and treatment.
Integrating Mental Health into Primary Care
Integrating mental health services into primary healthcare systems is crucial for improving access to care. This approach allows for early identification and management of mental health conditions within existing healthcare infrastructure, promoting a more holistic approach to health and well-being.
Taking care of your mental well-being is crucial, and remember, you absolutely have the right to protect your mental health; check out this resource: you have the right to protect your mental health. Prioritizing your mental health shouldn’t be seen as selfish, but rather as a necessary act of self-care. For those in Utah, World Mental Health Day is a great time to explore available resources, and you can find out who’s offering screenings by visiting this page: world mental health day who is offing screenings in utah.
Making use of these services is a sign of strength, not weakness.
Future Directions and Recommendations
Addressing the global mental health crisis requires a concerted effort from governments, healthcare providers, and individuals. Increased funding, improved workforce training, and enhanced service delivery are essential for achieving significant progress.
Key Steps for Improved Global Mental Health
A comprehensive plan for improved global mental health should prioritize increasing funding for mental health research, training, and service delivery. Strengthening the mental health workforce through education and training programs is vital. Implementing integrated mental health services into primary care systems is also crucial. Finally, reducing stigma and promoting mental health literacy through public awareness campaigns are essential components.
Recommendations for Policymakers, Providers, and Individuals
- Policymakers: Increase funding for mental health services, implement policies to reduce stigma, and integrate mental health into primary care.
- Healthcare Providers: Integrate mental health screening into routine care, provide evidence-based treatments, and advocate for policy changes.
- Individuals: Seek help when needed, challenge stigma, and promote mental health awareness.
Successful Community-Based Programs
Many successful community-based mental health programs exist, demonstrating the effectiveness of community-led initiatives. These programs often involve peer support, community education, and culturally appropriate interventions. Replicating successful models in diverse settings requires careful adaptation to local contexts and needs.
Impact of Socioeconomic Factors: World Health Organization 450 Million People Mental Health Disorders

Socioeconomic factors play a significant role in both the prevalence and outcome of mental health disorders. Poverty, inequality, and discrimination are strongly associated with increased risk and poorer outcomes.
Relationship Between Socioeconomic Factors and Mental Health
Poverty and inequality can create stressful living conditions that increase the risk of mental health problems. Lack of access to education, employment, and healthcare further exacerbates these challenges. Discrimination based on factors such as race, gender, or sexual orientation can also significantly impact mental well-being.
Societal Contributions to Stigma
Societal attitudes and beliefs contribute significantly to the stigma surrounding mental illness. Negative stereotypes, misinformation, and fear can lead to discrimination and social exclusion, hindering help-seeking behavior and recovery.
Taking care of your mental well-being is crucial, and remember, you absolutely have the right to protect your mental health; check out this resource: you have the right to protect your mental health. Prioritizing your mental health shouldn’t be seen as selfish, but rather as a necessary act of self-care. This is especially important during events like World Mental Health Day.
If you’re in Utah and looking for screenings, find out who’s offering them here: world mental health day who is offing screenings in utah. Early intervention and access to support are key to maintaining good mental health.
Addressing Socioeconomic Inequalities
Addressing socioeconomic inequalities is crucial for improving mental health outcomes. Policies aimed at reducing poverty, promoting social inclusion, and ensuring access to education, employment, and healthcare can significantly impact mental well-being. Investing in community-based programs that address social determinants of health is also vital.
The Role of Governments and NGOs
Governments and NGOs play complementary roles in addressing global mental health challenges. Governments bear the primary responsibility for providing mental healthcare services and supporting mental health initiatives, while NGOs often fill gaps in service provision and advocacy.
Government Responsibilities
Governments are responsible for establishing mental health policies, allocating resources for mental health services, training mental health professionals, and ensuring access to quality care. They also play a key role in raising awareness and reducing stigma through public health campaigns.
Contributions of NGOs
NGOs contribute significantly to global mental health efforts by providing direct services, conducting research, advocating for policy changes, and raising awareness. They often work in marginalized communities and address specific mental health needs, filling gaps in government services.
Comparative Approaches of Governments and NGOs
The approaches taken by governments and NGOs can vary significantly depending on their resources, priorities, and contextual factors. Governments typically focus on establishing national policies and frameworks, while NGOs often adopt more targeted and community-based approaches.
The global mental health crisis, affecting an estimated 450 million people, demands immediate and sustained action. While the challenge is immense, the progress made by the WHO and various organizations offers hope. By addressing systemic barriers, reducing stigma, and investing in evidence-based interventions, we can create a world where mental health support is accessible to all. The future requires a collaborative effort—governments, NGOs, healthcare providers, and individuals working together to build a more supportive and inclusive environment for those struggling with mental health disorders.
The journey towards improved global mental health is long, but with collective commitment, we can make significant strides towards a healthier future for all.
Share this content:
