Working with the Mental Health Population in Prison NYS
Working with the mental health population in prison NYS presents unique and significant challenges. The incarcerated population in New York State has a disproportionately high rate of mental illness compared to the general population, leading to complex issues in providing adequate care within the confines of a correctional facility. This necessitates a multifaceted approach involving specialized training for staff, innovative treatment programs, and a strong focus on successful reintegration into society upon release.
This exploration delves into the prevalence of mental illness within NYS prisons, examining the types of disorders most commonly diagnosed and comparing these rates to the broader state population. We’ll also analyze the obstacles to providing effective mental healthcare within prison settings, including resource limitations and the impact of the prison environment itself. Furthermore, we’ll review existing programs and initiatives, the crucial role of staff training, and the vital importance of post-release support and community-based resources.
Finally, we’ll consider legal and ethical considerations, compare approaches in other jurisdictions, and offer recommendations for improving mental healthcare within the NYS prison system.
The Prevalence of Mental Illness in NYS Prisons
Understanding the prevalence of mental illness within New York State’s prison system is crucial for developing effective treatment and support strategies. A significant portion of the incarcerated population struggles with mental health conditions, impacting their well-being, rehabilitation, and successful reintegration into society. This section details the statistical landscape of mental illness in NYS prisons, comparing it to the general population and identifying the most prevalent diagnoses.
Mental Health Diagnoses in NYS Prisons
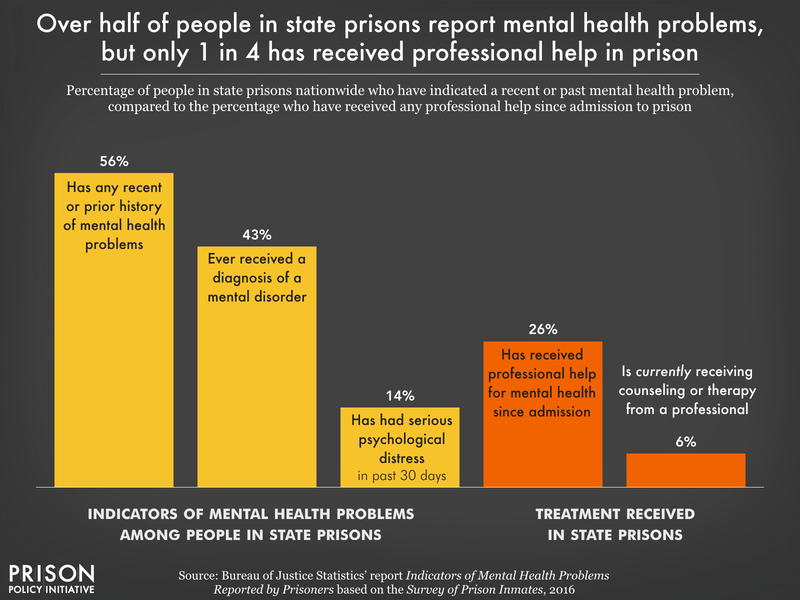
Studies consistently show a disproportionately high rate of mental illness among incarcerated individuals in New York State. While precise figures fluctuate based on data collection methods and reporting periods, a substantial percentage – estimates range from 50% to 70% – of the prison population has been diagnosed with at least one mental health condition. This significantly exceeds the prevalence rates observed in the general population of New York.
Types of Mental Illnesses
The most common mental health diagnoses within the NYS prison system include major depressive disorder, anxiety disorders (including generalized anxiety disorder, panic disorder, and post-traumatic stress disorder), schizophrenia, bipolar disorder, and substance use disorders (often co-occurring with other mental illnesses). The high prevalence of trauma-related disorders is particularly noteworthy, reflecting the often difficult life circumstances that precede incarceration.
Comparison to the General Population
The prevalence of mental illness among incarcerated individuals in NYS is considerably higher than in the general population of the state. While precise comparative statistics require careful analysis of data from various sources, the disparity is striking. This highlights the need for specialized mental healthcare services tailored to the unique needs and challenges faced by this population.
Setting achievable goals is key to improving mental well-being, and knowing how to write them effectively is crucial. Check out this helpful guide on writing measurable behavioral goals and objectives for mental health to learn practical strategies. It’s surprisingly easy to get lost in vague intentions, but clearly defined goals make a real difference. For example, while a hoodie like the you are bad for my mental health hoodie nihachu might be a fun statement, focusing on actionable steps towards better mental health provides much more lasting benefit.
Challenges in Providing Mental Healthcare in Prison Settings
Delivering effective mental healthcare within the confines of a prison presents numerous obstacles. These challenges stem from resource limitations, the inherent nature of the prison environment, and the complexities of managing mental health conditions within a highly structured and often stressful setting. This section explores these key difficulties.
Access to and Delivery of Mental Healthcare
Access to adequate mental healthcare services within NYS prisons is often limited by factors such as staffing shortages, long waiting lists for specialized care (e.g., psychiatric evaluations), and restricted access to certain treatments. The delivery of care is also complicated by the security protocols and logistical challenges inherent in a correctional setting. This can lead to delays in treatment, inadequate follow-up, and compromised treatment efficacy.
Resource Limitations
Effective mental healthcare requires sufficient funding, adequately trained personnel (psychiatrists, psychologists, social workers, nurses), and appropriate facilities. Resource limitations in NYS prisons often hinder the provision of comprehensive and timely care. Shortages of qualified mental health professionals are particularly problematic, leading to high caseloads and potentially compromised quality of care.
Impact of the Prison Environment
The prison environment itself can negatively impact mental health treatment outcomes. Factors such as overcrowding, violence, lack of privacy, and limited opportunities for therapeutic activities can exacerbate existing mental health conditions and impede recovery. The constant state of surveillance and restriction of movement can also be detrimental to mental well-being.
Current Mental Health Programs and Initiatives in NYS Prisons
Despite the challenges, New York State has implemented various programs and initiatives aimed at improving mental healthcare within its correctional facilities. This section provides an overview of these efforts, highlighting the types of interventions used and the roles of different healthcare professionals.
Overview of Existing Programs
The NYS Department of Corrections and Community Supervision (DOCCS) offers a range of mental health services, including medication management, individual and group therapy (cognitive behavioral therapy, dialectical behavior therapy are examples), and case management. Specialized units exist for individuals with severe mental illnesses, providing more intensive treatment. Programs focusing on substance abuse treatment are also integrated into the overall mental healthcare system, recognizing the high rates of co-occurring disorders.
Therapies and Interventions
A variety of therapeutic approaches are employed, ranging from medication management to various forms of psychotherapy. Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) are frequently used to address specific symptoms and develop coping mechanisms. Group therapy provides a supportive environment for sharing experiences and learning from others. In cases of severe mental illness, medication is often a crucial component of treatment.
Roles of Healthcare Professionals
A multidisciplinary team delivers mental healthcare in NYS prisons. Psychiatrists provide medication management and diagnosis. Psychologists conduct assessments, provide individual and group therapy, and may conduct specialized psychological testing. Social workers assist with case management, connecting individuals with resources, and providing support. Nurses play a vital role in medication administration and monitoring.
Setting achievable goals is crucial for mental well-being, and knowing how to write them effectively is key. Check out this guide on writing measurable behavioral goals and objectives for mental health to learn practical strategies. It’s surprisingly helpful, even if you’re not a therapist! Speaking of mental health, I saw a funny hoodie online, a you are bad for my mental health hoodie nihachu design, which made me chuckle.
It highlights how we sometimes need to acknowledge the little things that impact our mental state, both positively and negatively.
The Role of Staff Training and Education
Equipping correctional officers and other prison staff with the knowledge and skills to recognize and respond appropriately to mental health crises is paramount. Effective de-escalation techniques and crisis intervention strategies are essential for ensuring the safety and well-being of both staff and incarcerated individuals. This section explores the importance of comprehensive training and Artikels a hypothetical training module.
Importance of Staff Training
Training programs should equip staff with the ability to identify signs and symptoms of various mental health conditions, understand the impact of trauma, and implement effective de-escalation strategies. This knowledge is crucial for preventing crises, ensuring a safe environment, and facilitating access to appropriate mental health care.
Ideal Components of Training Programs
Comprehensive training programs should incorporate modules on mental health awareness, trauma-informed care, crisis intervention techniques, de-escalation strategies, communication skills, and cultural competency. Regular refresher training and ongoing professional development are also essential to maintain proficiency and adapt to evolving best practices.
Hypothetical Training Module: De-escalation and Crisis Intervention
A hypothetical training module could begin with an overview of common mental health conditions and their associated behaviors. It would then proceed to practical exercises on de-escalation techniques, including active listening, empathy, clear communication, and setting boundaries. Role-playing scenarios would simulate real-life situations, allowing trainees to practice their skills in a safe and controlled environment. Finally, the module would cover procedures for reporting and responding to serious mental health crises, emphasizing the importance of safety protocols.
Reintegration and Post-Release Support
Successful reintegration into the community is a significant challenge for individuals with mental illness leaving prison. Continued access to mental healthcare and robust community support systems are crucial for preventing relapse and promoting long-term stability. This section discusses the challenges and strategies for supporting successful reintegration.
Challenges Faced Upon Release
Individuals with mental illness often face significant obstacles upon release, including lack of housing, limited access to healthcare, unemployment, and social isolation. These factors can increase the risk of relapse and recidivism. The transition from the structured environment of prison to the complexities of community life can be particularly difficult for those with pre-existing mental health conditions.
Strategies for Smooth Transition
Strategies for ensuring a smooth transition include providing access to continued mental healthcare, connecting individuals with supportive housing, assisting with job placement, and facilitating access to social support networks. Pre-release planning and coordination with community-based organizations are essential for establishing a support system before release.
Importance of Community-Based Resources
Community-based mental health services play a vital role in successful reintegration. These services provide ongoing treatment, support, and resources that help individuals maintain stability and avoid relapse. Collaboration between correctional facilities and community organizations is essential to create a seamless continuum of care.
Legal and Ethical Considerations
Providing mental healthcare in prison settings raises important legal and ethical considerations. Respecting the rights of incarcerated individuals with mental illness, ensuring informed consent, and maintaining patient confidentiality are crucial aspects of ethical practice. This section explores these key considerations.
Key Legal and Ethical Considerations, Working with the mental health population in prison nys
The legal rights of incarcerated individuals with mental illness are protected under various laws and regulations. These rights include access to adequate medical and mental healthcare, treatment in the least restrictive environment possible, and the right to refuse treatment (with some exceptions). Ethical considerations emphasize the importance of providing care that is respectful, compassionate, and culturally sensitive.
Rights of Incarcerated Individuals
Incarcerated individuals retain many of the same rights as individuals in the community, including the right to privacy, due process, and freedom from cruel and unusual punishment. These rights are particularly relevant when considering the provision of mental healthcare, ensuring that treatment is provided ethically and legally.
Informed Consent and Confidentiality
Informed consent is a cornerstone of ethical mental healthcare. Individuals must be provided with clear and understandable information about their diagnosis, treatment options, and potential risks and benefits before consenting to treatment. Maintaining patient confidentiality is also crucial, although this may be subject to limitations imposed by security and legal requirements within the prison setting.
Comparative Analysis of Mental Health Care in Other Jurisdictions
Examining mental healthcare systems in other jurisdictions can reveal best practices and potential areas for improvement within the NYS prison system. This section offers a comparative analysis, highlighting key differences and potential avenues for reform.
Comparison with Other States/Countries
Some jurisdictions have implemented innovative approaches to prison mental healthcare, such as specialized mental health courts, increased access to medication-assisted treatment, and greater emphasis on trauma-informed care. Comparisons with these systems can highlight areas where NYS could improve its own approach. For example, Norway’s focus on rehabilitation and community reintegration, or certain European countries’ emphasis on restorative justice, offer valuable lessons.
Best Practices from Other Jurisdictions
Best practices from other jurisdictions include implementing comprehensive mental health screening upon entry, providing timely access to specialized mental health services, utilizing evidence-based treatment modalities, and fostering collaboration between correctional facilities and community-based organizations. These practices could be adapted and implemented within the NYS system to enhance the quality of care.
Structured Comparison
A structured comparison might involve analyzing different aspects of mental healthcare across jurisdictions, such as staffing levels, funding models, types of treatment offered, and recidivism rates among individuals with mental illness. This analysis could reveal key differences and identify areas where NYS could benefit from adopting best practices observed elsewhere.
Recommendations for Improvement: Working With The Mental Health Population In Prison Nys
Improving mental healthcare services in NYS prisons requires a multifaceted approach encompassing policy changes, increased resource allocation, and implementation of evidence-based practices. This section Artikels actionable recommendations prioritized by their potential impact and feasibility.
Actionable Recommendations
- Increase funding for mental health services within NYS prisons to address staffing shortages and improve access to care.
- Implement comprehensive mental health screening upon entry into the correctional system to identify individuals requiring treatment.
- Expand access to evidence-based treatment modalities, such as CBT and DBT, and medication-assisted treatment for substance use disorders.
- Develop and implement standardized training programs for correctional officers and other prison staff on mental health awareness, de-escalation techniques, and crisis intervention.
- Strengthen collaboration between correctional facilities and community-based mental health organizations to ensure a seamless continuum of care upon release.
- Develop and implement programs focusing on trauma-informed care to address the high prevalence of trauma among incarcerated individuals.
- Invest in research to evaluate the effectiveness of current mental health programs and identify areas for improvement.
Prioritization and Implementation
The recommendations above should be prioritized based on their potential impact and feasibility. A phased implementation approach, starting with readily achievable steps, would ensure sustainable improvements over time. Each recommendation should be accompanied by a detailed implementation plan outlining specific steps, timelines, and resource requirements.
Effectively addressing the mental health needs of the incarcerated population in New York State requires a comprehensive and collaborative effort. From improved staff training and increased resources to enhanced reintegration support and a commitment to ethical and legal best practices, significant advancements are needed. By learning from other jurisdictions and prioritizing evidence-based approaches, we can strive towards a system that not only treats mental illness but also promotes healing, recovery, and successful reintegration into society, ultimately fostering safer and healthier communities.
Share this content:

