Lupus medication plays a crucial role in managing this complex autoimmune disease. Lupus, an inflammatory condition that can affect various organs, often requires a combination of therapies to control symptoms and prevent complications. This article explores the different types of medications used to treat lupus, their mechanisms of action, and the considerations involved in choosing the right treatment plan.
From immunosuppressants that dampen the immune system’s overactivity to anti-inflammatories that reduce inflammation, the medications used to treat lupus are designed to target specific aspects of the disease. Understanding the various treatment options and their potential benefits and risks is essential for patients to make informed decisions about their care.
Lupus Medication Overview
Lupus is a chronic autoimmune disease that can affect various organs and systems in the body. The immune system, which normally protects the body from foreign invaders like bacteria and viruses, mistakenly attacks healthy tissues. This leads to inflammation, pain, and damage in affected areas.
Lupus can manifest in different ways, making diagnosis challenging.
Common Lupus Medications
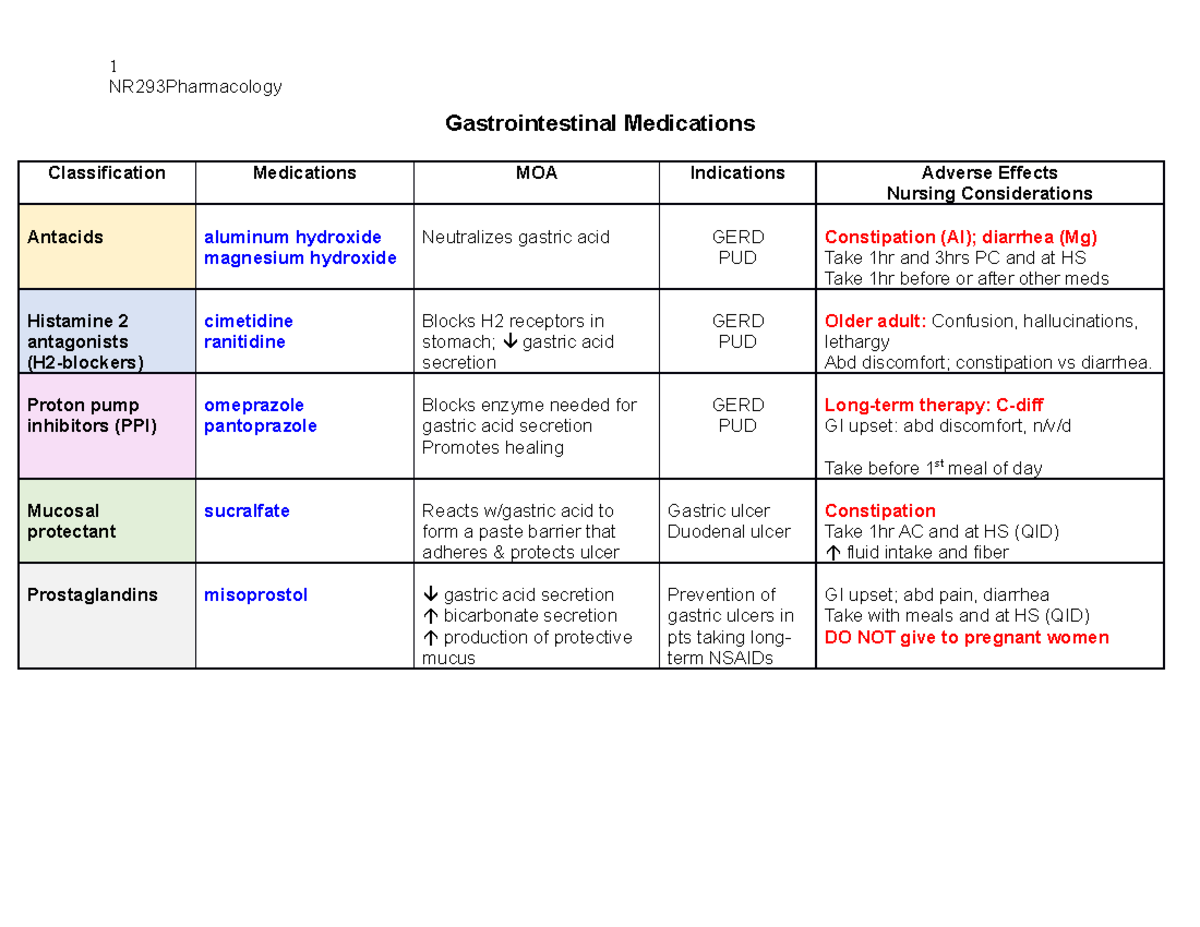
A wide range of medications are used to manage lupus symptoms and prevent disease progression. These medications fall into different categories, each targeting specific aspects of the disease. Here’s a breakdown of common lupus medications and their mechanisms of action:
- Immunosuppressants: These medications suppress the immune system’s activity, reducing its attacks on healthy tissues. Common examples include:
- Methotrexate (Trexall, Rheumatrex): This medication is often used for mild to moderate lupus, particularly for joint inflammation. It works by interfering with the production of certain immune cells.
If you’re experiencing a urinary tract infection (UTI), it’s important to seek medical advice. Your doctor can prescribe the right urinary tract infection medication for your specific situation. This could be antibiotics, pain relievers, or other treatments. Remember, self-treating a UTI can be dangerous, so always consult a healthcare professional.
- Azathioprine (Imuran): This medication is used for more severe lupus, often in combination with other immunosuppressants. It blocks the production of immune cells, slowing down the immune response.
- Cyclophosphamide (Cytoxan): This medication is reserved for severe lupus, particularly when other treatments have failed.
It suppresses the immune system by killing rapidly dividing cells, including immune cells.
- Mycophenolate Mofetil (CellCept): This medication is used for lupus nephritis (kidney inflammation) and other severe forms of lupus. It blocks the production of certain immune cells involved in the inflammatory process.
- Methotrexate (Trexall, Rheumatrex): This medication is often used for mild to moderate lupus, particularly for joint inflammation. It works by interfering with the production of certain immune cells.
- Anti-Inflammatories: These medications reduce inflammation and pain, providing relief from lupus symptoms. Common examples include:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These over-the-counter medications like ibuprofen (Advil, Motrin) and naproxen (Aleve) are often used for mild to moderate pain and inflammation.
- Corticosteroids: These medications, such as prednisone, are powerful anti-inflammatories used for more severe lupus symptoms or flare-ups.
They can be taken orally, injected, or applied topically.
- Pain Relievers: These medications are used to manage pain associated with lupus, particularly in the joints and muscles. Common examples include:
- Acetaminophen (Tylenol): This over-the-counter medication is effective for mild to moderate pain, but it doesn’t have anti-inflammatory properties.
- Opioids: These medications, such as oxycodone and hydrocodone, are prescribed for severe pain that doesn’t respond to other medications.
They are typically used for short periods due to their potential for addiction.
- Antimalarials: These medications, such as hydroxychloroquine (Plaquenil), are used to treat lupus symptoms, particularly skin and joint inflammation. Their exact mechanism of action is unclear, but they are thought to suppress the immune system and reduce inflammation.
- Biologics: These newer medications target specific proteins involved in the immune system’s attack on healthy tissues. They are used for severe lupus, particularly when other treatments have failed. Examples include:
- Belimumab (Benlysta): This medication targets a protein called B lymphocyte stimulator (BLyS), which is involved in the activation of immune cells.
- Rituximab (Rituxan): This medication targets B cells, a type of immune cell that produces antibodies that can attack healthy tissues in lupus.
Treatment Strategies and Considerations, Lupus medication
Lupus treatment involves a combination of medications and lifestyle modifications tailored to the individual patient’s needs. Treatment goals include controlling symptoms, preventing organ damage, and improving quality of life.
- Medication Combinations: Often, multiple medications are used together to effectively manage lupus symptoms. For example, a patient might take an immunosuppressant to suppress the immune system, a corticosteroid to reduce inflammation, and an antimalarial to manage skin and joint symptoms.
- Lifestyle Modifications: Along with medication, lifestyle changes can play a significant role in managing lupus. These may include:
- Stress Management: Stress can trigger lupus flares, so finding healthy ways to manage stress, such as exercise, relaxation techniques, or therapy, is important.
If you’re experiencing a urinary tract infection (UTI), you might be wondering about the best treatment options. Fortunately, there are several effective medications available, such as antibiotics, to help clear up the infection. You can learn more about these medications and their potential side effects by visiting this helpful resource: urinary tract infection medication.
Remember to always consult your doctor before starting any new medication, especially if you have any underlying health conditions.
- Sun Protection: Sun exposure can worsen lupus symptoms, so protecting your skin from the sun with sunscreen, protective clothing, and avoiding prolonged sun exposure is crucial.
- Healthy Diet: Eating a balanced diet with plenty of fruits, vegetables, and whole grains can support overall health and help manage lupus symptoms.
- Regular Exercise: Moderate exercise can improve physical fitness, reduce fatigue, and help manage lupus symptoms.
- Smoking Cessation: Smoking can worsen lupus symptoms and increase the risk of complications.
- Stress Management: Stress can trigger lupus flares, so finding healthy ways to manage stress, such as exercise, relaxation techniques, or therapy, is important.
- Medication Selection Factors: Several factors influence the choice of lupus medications, including:
- Severity of Symptoms: More severe lupus symptoms may require stronger medications, such as immunosuppressants or biologics.
- Individual Patient Characteristics: Factors such as age, overall health, and other medical conditions can influence medication choices.
- Potential Side Effects: All medications have potential side effects, and doctors must weigh the benefits of treatment against the risks.
- Treatment Options Comparison: Different treatment options have varying advantages and disadvantages:
- Efficacy: Some medications are more effective than others for specific lupus symptoms or types of lupus.
- Safety Profiles: Medications have different safety profiles, with some having more potential side effects than others.
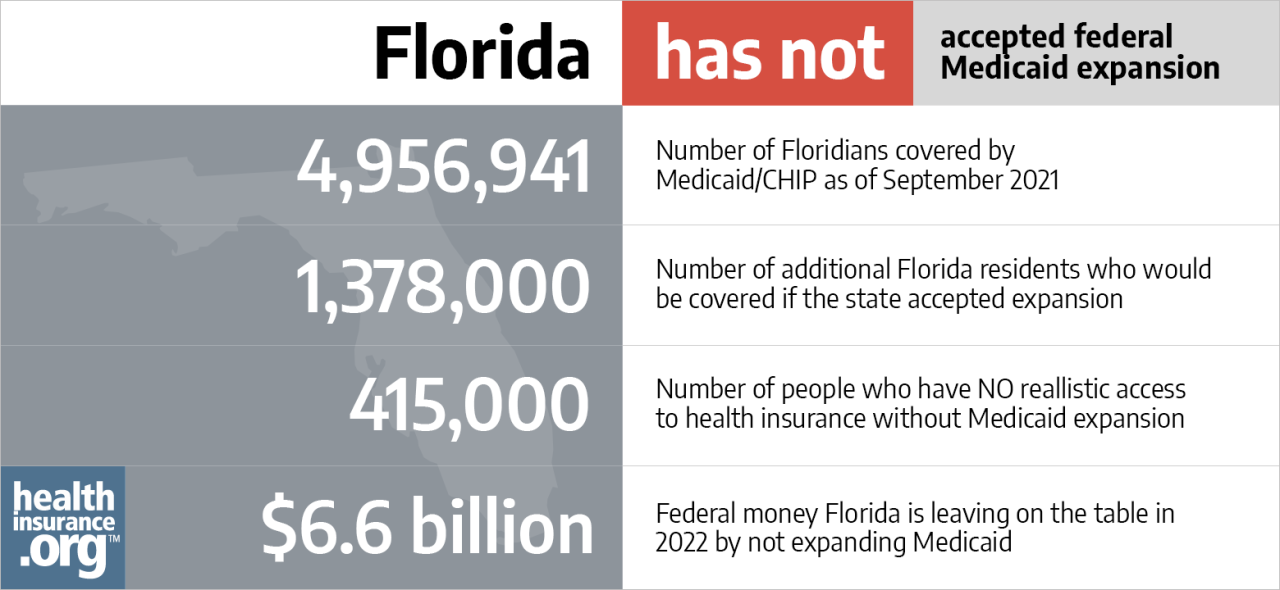
- Cost Considerations: The cost of lupus medications can vary significantly, and some medications may not be covered by insurance.
Managing Lupus Medications

Managing lupus medications effectively is essential for controlling symptoms and preventing disease progression. Here’s a guide for patients:
- Proper Storage: Store medications as directed by the pharmacist or healthcare provider. This may include storing them at room temperature, in a cool and dry place, or in the refrigerator.
- Administration: Follow your healthcare provider’s instructions carefully regarding how to take your medications. This includes the dosage, frequency, and timing of administration.
- Adherence Strategies: Taking your medications as prescribed is crucial for effective treatment. Use reminders, pill organizers, or a medication tracking app to help you stay on schedule.
- Regular Monitoring: Regular follow-up appointments with your healthcare provider are essential to monitor your progress, adjust medications as needed, and address any potential side effects.
- Managing Side Effects: All medications have potential side effects, and it’s important to report any unusual symptoms to your healthcare provider. They can help you manage side effects and adjust your medications if necessary.
- Promoting Medication Adherence: Building a strong relationship with your healthcare provider, understanding your treatment plan, and being actively involved in your care can help improve medication adherence.
Research and Development in Lupus Medication
Research and development efforts in lupus medication are ongoing, with a focus on developing new and improved treatment options.
- Emerging Treatment Options: Researchers are investigating new therapies that target specific pathways involved in lupus, such as:
- Targeted Therapies: These medications target specific proteins or cells involved in the immune system’s attack on healthy tissues.
- Gene Therapy: This approach involves modifying genes to correct the underlying genetic defects that contribute to lupus.
- Stem Cell Therapy: This therapy involves using stem cells to regenerate healthy tissues and potentially restore immune function.
- Challenges and Opportunities: Developing new lupus medications faces several challenges, including:
- Complexity of the Disease: Lupus is a complex autoimmune disease with multiple causes and manifestations, making it difficult to develop therapies that target all aspects of the disease.
- Limited Understanding of the Disease: Despite progress, scientists still have much to learn about the underlying mechanisms of lupus, which hampers the development of effective treatments.
- Clinical Trial Challenges: Conducting clinical trials for lupus medications is challenging due to the chronic nature of the disease and the variability in its presentation.
- Future Directions: Future research in lupus medication is likely to focus on:
- Personalized Medicine: Tailoring treatment plans to individual patients based on their genetic makeup and other factors.
- Prevention Strategies: Identifying and targeting the early stages of lupus to prevent disease progression.
- Improved Drug Delivery: Developing new drug delivery systems that enhance the effectiveness and safety of lupus medications.
Final Review
Living with lupus can be challenging, but with the right treatment plan and a collaborative relationship with healthcare professionals, patients can manage their symptoms, improve their quality of life, and achieve long-term remission. By staying informed about lupus medication and its management, individuals can empower themselves to take an active role in their health journey.
Remember, consistent communication with your doctor is key to tailoring treatment and ensuring the best possible outcomes.