Why Was 1996s Mental Health Parity Introduced?
Why was the mental health parity in 1996 introduced? This question delves into a pivotal moment in American healthcare history, a time when the disparity between mental and physical health coverage was starkly evident. The Mental Health Parity Act of 1996, though imperfect, represented a significant step towards addressing long-standing inequalities and societal stigma surrounding mental illness. This journey involved decades of advocacy, shifting political landscapes, and a growing understanding of the profound impact of mental health on individuals and society as a whole.
The Act’s introduction was fueled by a confluence of factors: increasing awareness of mental health issues, persistent lobbying efforts by advocacy groups, and a growing recognition of the economic burden of untreated mental illness. The legislation aimed to level the playing field, ensuring that insurance coverage for mental health treatment mirrored that of physical health, a concept that had been previously largely ignored.
However, the Act’s initial implementation wasn’t without its challenges and limitations, leading to ongoing debates and subsequent legislation aimed at strengthening and expanding mental health parity.
It’s a crazy situation, isn’t it? You can easily find information on the stark realities of you can buy a gun but not mental health access in many places, highlighting a serious imbalance in resource allocation. This disparity is especially concerning when considering the struggles faced by women in South Africa. The article on women mental health south africa every woman lily-rose-mlisa sheds light on the unique challenges they face and the need for better support systems.
We need to address both issues urgently for a healthier and safer society.
The Political Climate and the Mental Health Parity Act of 1996
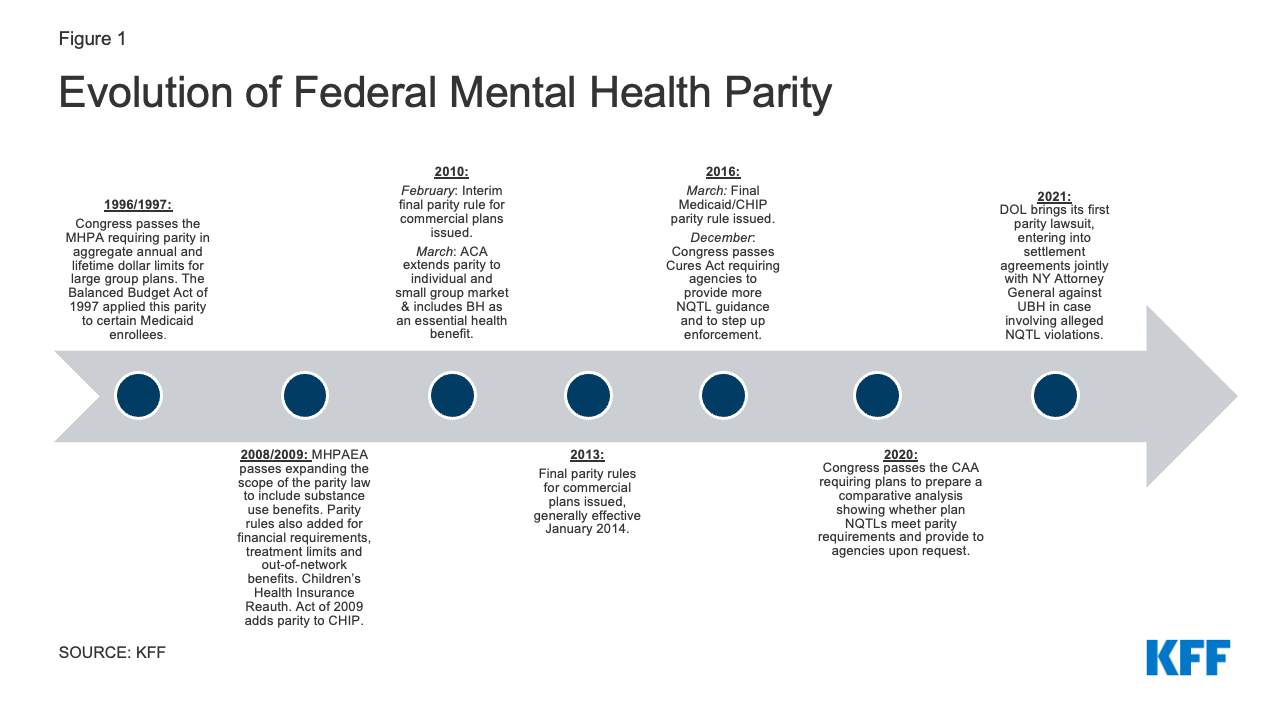
The Mental Health Parity Act of 1996 marked a significant turning point in the recognition and treatment of mental illness in the United States. Its passage was the culmination of years of advocacy, shifting societal attitudes, and strategic political maneuvering. Understanding the context surrounding its introduction is crucial to grasping its impact and limitations.
Societal Attitudes Towards Mental Illness Before 1996
In the years leading up to 1996, societal attitudes towards mental illness were often characterized by stigma, misunderstanding, and a lack of awareness. Mental health conditions were frequently shrouded in secrecy, leading to underdiagnosis, undertreatment, and significant societal discrimination against those affected. Many people with mental illnesses faced significant barriers to accessing appropriate care, often due to financial constraints and the lack of adequate insurance coverage.
This resulted in a significant gap between the need for mental healthcare services and the availability of such services. The prevailing belief that mental illness was a personal failing rather than a treatable medical condition further exacerbated the problem.
Advocacy Efforts and Political Influence
The passage of the MHPA was significantly influenced by the tireless advocacy of mental health organizations and individual activists. Groups like the National Alliance on Mental Illness (NAMI) played a pivotal role in raising public awareness, lobbying Congress, and building support for legislative change. These organizations highlighted the disparities in insurance coverage for mental health compared to physical health, effectively framing the issue as one of fairness and equity.
Key political figures, recognizing the growing public concern and the potential for electoral gains, played a critical role in pushing the legislation through Congress. While specific individuals and their exact influence requires further research into legislative records, the overall political climate was receptive to addressing this critical health disparity.
Key Provisions and Limitations of the 1996 Act
The Mental Health Parity Act of 1996 aimed to address the inequities in insurance coverage between mental health and substance abuse treatment and physical healthcare. However, its initial impact was limited by several key provisions and loopholes.
It’s a frustrating reality that accessing mental healthcare can be a struggle. The article, you can buy a gun but not mental health , highlights this disparity perfectly. This issue is especially pertinent in South Africa, where the mental health needs of women are often overlooked. Read more about the challenges faced by women in South Africa and the important work of Lily-Rose Mlisa in this piece: women mental health south africa every woman lily-rose mlisa.
It’s crucial to advocate for better access and reduce the stigma surrounding mental health services.
Specific Requirements and Comparisons
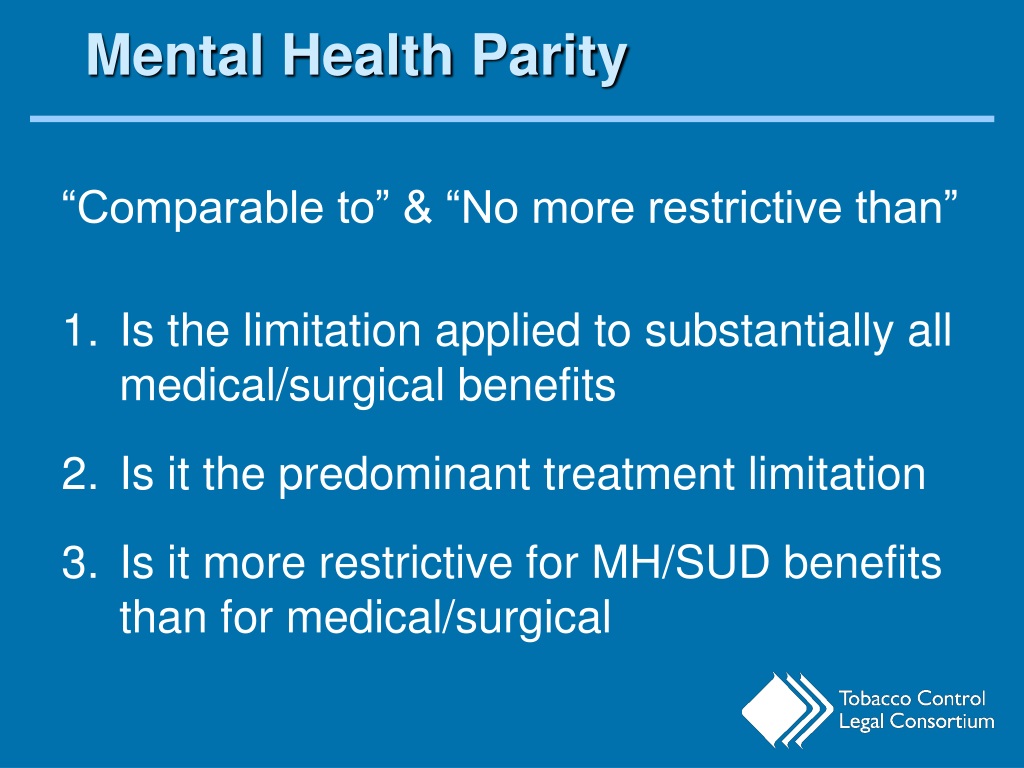
The Act mandated that group health plans offering mental health and substance abuse benefits could not impose stricter limits on those benefits than those imposed on medical and surgical benefits. This meant that limitations on the number of visits, days of treatment, or the amount of money spent on mental health care could not be more restrictive than those for physical health conditions.
However, it did not require plans to offer mental health benefits in the first place, leaving many individuals still without coverage. The comparison to physical illness coverage was intended to establish a baseline of equitable treatment, but the Act fell short of ensuring equal access.
Limitations and Loopholes
The 1996 Act contained significant loopholes. For example, it didn’t apply to smaller employers, leaving a substantial portion of the workforce uncovered. Moreover, the definition of “parity” was not clearly defined, allowing insurers to find ways to limit benefits through other means, such as high co-pays, deductibles, or restrictive network restrictions. These loopholes severely diminished the effectiveness of the legislation in achieving its intended goal of true parity in mental health coverage.
The Impact and Subsequent Legislation
While the 1996 MHPA had some positive impacts, it was far from a complete solution. Its limitations led to further legislative action.
Immediate and Long-Term Effects
The immediate effects of the Act were modest. Some individuals gained access to improved mental health coverage, while others saw little change. The long-term consequences, however, were more significant. The Act laid the groundwork for future legislation and helped raise public awareness about the importance of mental health parity. It created a momentum that eventually led to more comprehensive reforms.
Changes in insurance coverage and treatment availability were gradual and varied significantly depending on the individual’s employer and insurance plan.
Subsequent Legislation
The limitations of the 1996 Act spurred further legislative efforts. Subsequent legislation, notably the Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA) and its subsequent amendments, significantly expanded coverage and addressed many of the loopholes present in the original Act. The MHPAEA eliminated many of the exceptions and clarified the definition of parity, leading to more substantial improvements in access to mental healthcare.
The comparison between the 1996 Act and later legislation highlights the evolution of policy and a growing understanding of the complexities of ensuring equitable access to mental healthcare.
Economic Considerations: Why Was The Mental Health Parity In 1996 Introduced
The economic arguments surrounding the MHPA were complex and often conflicting.
Arguments For and Against Parity, Why was the mental health parity in 1996 introduced
Proponents argued that providing parity in mental health coverage would lead to better health outcomes, reduced healthcare costs in the long run (due to early intervention and prevention), and increased productivity. Opponents, however, expressed concerns about the potential cost increases for insurance companies and employers. They argued that the increased demand for mental health services would strain the healthcare system and lead to higher premiums.
The economic debate highlighted the tension between the social benefits of parity and the financial implications for stakeholders.
Financial Implications
The financial implications for insurance companies and employers were significant. While some studies showed that increased access to mental health services could lead to cost savings in the long term, the immediate costs of expanding coverage were undeniable. The cost-benefit analysis was complex and depended on various factors, including the specific design of insurance plans, the prevalence of mental illness in the covered population, and the effectiveness of treatment interventions.
Insurance Company Perspectives and Challenges
Insurance companies played a crucial role in implementing the MHPA, facing significant challenges in the process.
Challenges and Adaptations
Insurance companies faced several challenges in complying with the Act’s provisions. These included adapting their policies and procedures to ensure that mental health benefits were treated equitably with medical and surgical benefits, dealing with increased demand for mental health services, and managing the costs associated with expanded coverage. They had to adjust their networks of providers, update their claims processing systems, and develop new strategies for managing utilization and costs.
Insurance Company Perspectives
The perspective of insurance companies on the Act’s impact was mixed. While some companies viewed the Act as a necessary step towards improving healthcare equity, others expressed concerns about its financial implications. Many companies actively sought ways to comply with the law while minimizing their financial burden. This involved a variety of strategies, including negotiating lower rates with providers, implementing utilization management programs, and focusing on preventive care to reduce the overall cost of mental health services.
Patient Experiences Before and After the Act
The experiences of individuals seeking mental healthcare before and after the MHPA varied widely.
Changes in Access and Affordability
Before the Act, many individuals struggled to access affordable mental healthcare due to limited insurance coverage and high out-of-pocket costs. The Act, while imperfect, did lead to improvements in access for some individuals, particularly those with employer-sponsored insurance plans that expanded their coverage to meet the new requirements. However, many others continued to face significant barriers to care, particularly those with limited or no insurance coverage, or those living in areas with limited access to mental health providers.
The impact on quality and affordability varied widely based on factors such as geographic location, insurance coverage, and the type of mental health service needed.
Demographic Variations
The impact of the Act varied across different demographic groups. Individuals from lower socioeconomic backgrounds, racial and ethnic minorities, and those in rural areas often continued to experience greater barriers to access than their more privileged counterparts. The Act did not fully address the underlying social determinants of health that contribute to disparities in mental health care access and outcomes.
The Ongoing Debate on Mental Health Parity
The debate on mental health parity continues, highlighting the ongoing need for legislative improvements.
Areas Needing Further Action
Despite significant progress, significant gaps remain in achieving comprehensive mental health parity. Further legislative action is needed to address issues such as the continued high cost of mental health services, inadequate access to care in underserved communities, and the need for improved integration of mental health services with physical healthcare. Addressing these challenges requires a multifaceted approach that includes not only legislative reforms but also improvements in the availability of mental health professionals, expansion of community-based mental health services, and efforts to reduce the stigma surrounding mental illness.
Framework for Future Legislation
A potential framework for future legislation should focus on strengthening existing parity laws, expanding coverage to include a wider range of mental health services, and addressing the underlying social determinants of health that contribute to disparities in mental health care. This could involve increasing funding for mental health services, expanding the workforce of mental health professionals, and implementing policies to improve access to care in underserved communities.
Furthermore, future legislation should prioritize the development of comprehensive, integrated healthcare systems that seamlessly integrate mental health and physical health care, ensuring that individuals receive the holistic care they need.
The Mental Health Parity Act of 1996 marked a watershed moment, signifying a societal shift in how mental illness was perceived and addressed. While not a perfect solution, it laid the groundwork for future improvements in access to mental healthcare. The journey toward true parity continues, requiring ongoing legislative action, increased public awareness, and a commitment to dismantling the stigma that continues to hinder individuals from seeking the help they need.
The legacy of the 1996 Act serves as a reminder of the importance of persistent advocacy and the ongoing need for comprehensive mental health reform.
Share this content:
