Why Refer to Urgent Mental Health Services?
Why would a provider refer to mental health urgent services? This crucial question delves into the complex interplay of risk assessment, symptom severity, resource availability, and ethical considerations. Understanding the factors that prompt an urgent referral is vital for ensuring timely and effective care for individuals experiencing a mental health crisis. This exploration will illuminate the decision-making process involved, highlighting the provider’s role in safeguarding patient well-being.
Providers face the challenging task of discerning when a patient’s needs surpass the scope of routine care. This involves careful evaluation of immediate risks, the intensity of symptoms, and access to appropriate resources. The decision to refer is not taken lightly and often involves navigating legal and ethical guidelines while prioritizing the patient’s safety and well-being. This process requires a nuanced understanding of both the patient’s situation and the available mental health services.
Understanding Urgent Mental Health Referrals: Why Would A Provider Refer To Mental Health Urgent Services
Providers refer patients to urgent mental health services when immediate intervention is necessary to address a significant risk to the individual or others. This decision involves careful assessment of various factors, including the severity of symptoms, access to care, and ethical considerations. This article Artikels the key considerations guiding such referrals.
Thinking about a career in public service? Jobs with the state of Texas often offer fulfilling work, and if you’re interested in mental health, check out the opportunities available at working for the state of Texas mental health services. It’s a demanding but rewarding field. The pressure on professionals isn’t limited to state jobs, though; research shows significant mental health challenges among academics, particularly PhD students, as highlighted in this study on work organization and mental health problem in PhD students.
Both fields require resilience and support systems to navigate the inherent stresses.
Immediate Risk Assessment: Reasons for Urgent Referral, Why would a provider refer to mental health urgent services
Providers use established criteria to assess immediate risk. This involves evaluating the patient’s potential for self-harm or harm to others, considering their history, current behavior, and expressed intentions. Specific behaviors like expressing suicidal ideation with a plan, exhibiting severe aggression towards others, or engaging in self-injurious behavior trigger urgent referrals. A delay in care in these situations could lead to tragic consequences, such as suicide attempts or violent acts.
Thinking about a career in public service? Jobs with the state of Texas often offer fulfilling work, and the mental health field is particularly rewarding. Check out this resource on working for the state of Texas mental health services to learn more about opportunities. It’s important to remember that maintaining good mental health is crucial in any career, especially demanding ones.
For instance, research shows a strong correlation between work organization and mental well-being, particularly for PhD students, as highlighted in this study on work organization and mental health problem in PhD students. Prioritizing well-being is key to success in any field.
- Criteria include a detailed history of self-harm or violence.
- Specific behaviors like expressing a detailed suicide plan or actively threatening harm to others are immediate red flags.
- Examples of situations demanding immediate intervention include a patient expressing an intent to harm themselves with readily available means, or a patient exhibiting uncontrollable rage towards family members.
Severity of Mental Health Symptoms: Indicators of Urgency
The severity of mental health symptoms plays a crucial role in determining the urgency of a referral. Symptoms like severe psychosis, acute mania, or a sudden and significant worsening of depression necessitate immediate intervention. These symptoms often represent a departure from the patient’s baseline functioning, indicating a need for specialized, immediate care.
- Symptoms like severe hallucinations, delusions, or disorganized thinking are indicators of urgent need.
- Manageable symptoms are those that can be addressed through routine therapy and medication management, while urgent symptoms demand immediate intervention to prevent harm.
- Escalating symptoms, such as increasing self-harm behaviors or escalating suicidal ideation, warrant immediate referral.
Lack of Access to Care: Referral for Timely Intervention
Geographical location and financial constraints can significantly impact access to mental health services. Providers often refer patients to urgent care when local resources are limited or unavailable. This ensures patients receive timely intervention, even if it requires navigating challenges in access.
- Challenges include long waiting lists for appointments, limited availability of specialized services, and lack of affordable treatment options.
- Situations where limited resources necessitate urgent referral include a patient living in a rural area with no access to mental health professionals or a patient lacking insurance coverage for necessary care.
- The referral process involves identifying available urgent care options, contacting the facility to arrange admission, and coordinating transportation for the patient.
Patient’s Safety and Well-being: Prioritizing Urgent Needs
Patient safety and well-being are paramount in referral decisions. Providers employ a risk assessment framework that balances the potential for harm with the patient’s autonomy. Ethical considerations ensure the referral is in the patient’s best interest, while adhering to legal and professional standards.
- A framework for evaluation includes assessing the immediacy of the risk, the severity of the symptoms, and the availability of resources.
- Ethical considerations include respecting patient autonomy while ensuring their safety and well-being.
- Prioritizing urgent needs involves weighing the potential benefits of intervention against potential risks and side effects of treatment.
The Role of the Referring Provider: Facilitating Smooth Transitions
The referring provider plays a vital role in ensuring a smooth transition to urgent care. This involves clear communication with the urgent care team, secure transfer of patient information, and follow-up to support continuous care. Effective communication minimizes delays and potential disruptions in treatment.
- Actions include providing a comprehensive summary of the patient’s history, current symptoms, and treatment plan.
- Best practices for communication include using a secure electronic health record system to share information and establishing clear communication channels with the urgent care team.
- A communication protocol should include a secure method for exchanging sensitive patient information, such as protected health information (PHI).
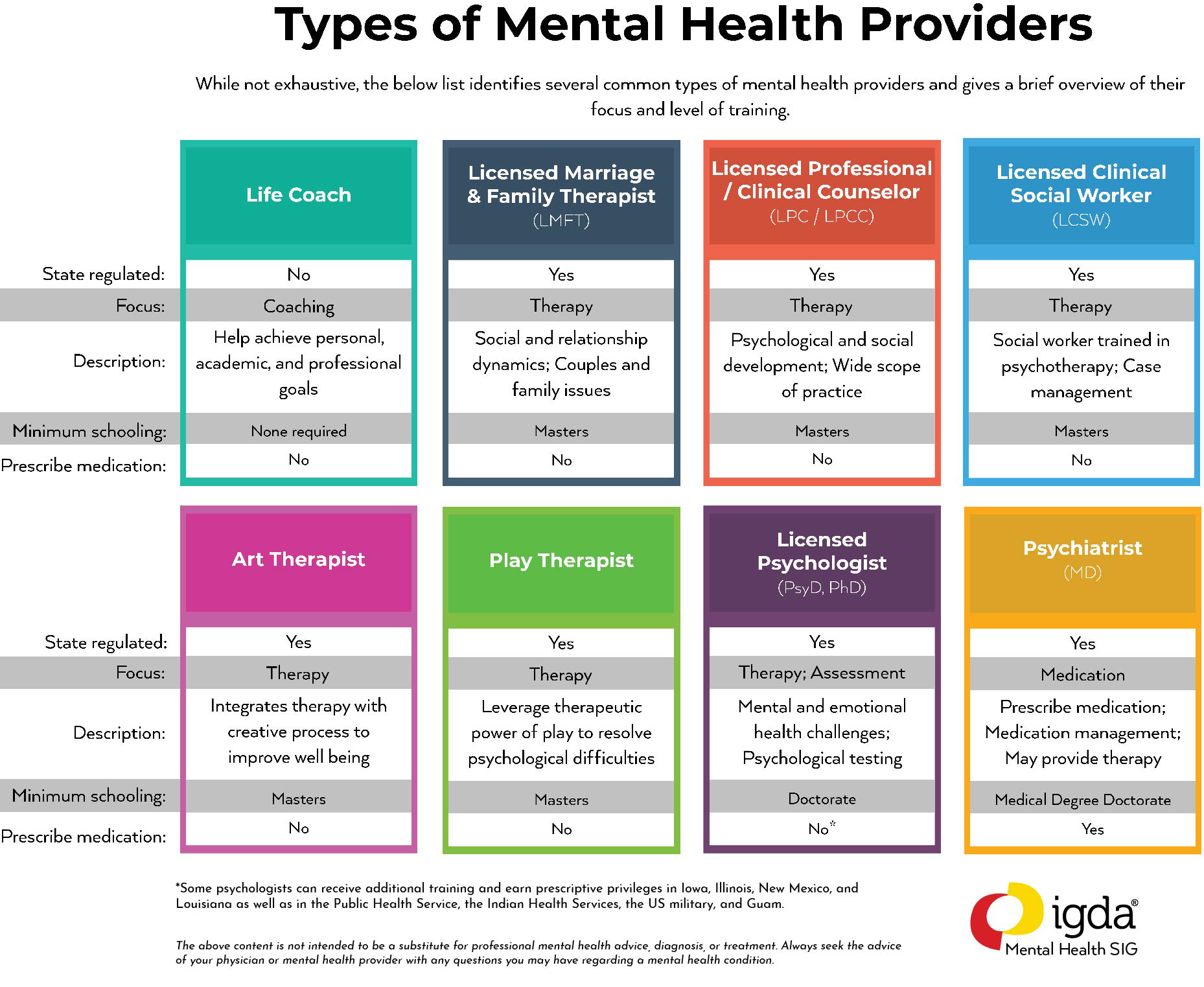
Types of Urgent Mental Health Services: Understanding Available Options
Urgent mental health services encompass various levels of care, from crisis hotlines and walk-in clinics to inpatient hospitalization. The choice of service depends on the patient’s specific needs and the severity of their condition. Matching the patient’s needs to the appropriate level of care is critical for effective treatment.
- Services include crisis hotlines, walk-in clinics, emergency rooms, inpatient psychiatric units, and mobile crisis teams.
- Levels of care range from brief interventions to extended hospitalization, depending on the severity of the patient’s condition.
- Matching patient needs involves assessing the risk level, symptom severity, and the availability of resources.
Legal and Ethical Considerations: Guiding Referral Decisions
Providers must adhere to legal and ethical guidelines when making urgent referrals. This includes mandatory reporting requirements in cases of suspected child abuse or neglect, and ensuring patient confidentiality while prioritizing their safety. A decision-making framework that integrates these considerations is essential.
- Legal responsibilities include adherence to state and federal laws regarding mandatory reporting and patient confidentiality.
- Mandatory reporting is required when there is reasonable suspicion of child abuse, elder abuse, or neglect.
- A decision-making framework integrates legal requirements with ethical principles to ensure responsible and ethical referrals.
Post-Referral Follow-up: Ensuring Continuous Care
Post-referral follow-up is crucial for ensuring continuous care and monitoring patient progress. Tracking patient progress after an urgent referral helps the referring provider to evaluate the effectiveness of the intervention and adjust the treatment plan as needed. This coordinated approach ensures a smoother transition back to routine care.
- The importance of follow-up includes monitoring the patient’s response to treatment, identifying any potential complications, and coordinating ongoing care.
- A system for tracking progress might involve regular phone calls, scheduled appointments, or collaboration with the urgent care team.
- The referring provider’s role includes coordinating ongoing care, ensuring smooth transitions, and providing support to the patient and their family.
Building Trust and Rapport: Communicating Effectively with Patients
Effective communication is key to building trust and encouraging patient cooperation during urgent referrals. Sensitive information must be conveyed with empathy and respect, addressing patient concerns and anxieties. A collaborative approach fosters a positive therapeutic alliance.
- Strategies include using clear and concise language, providing explanations in a non-judgmental manner, and actively listening to patient concerns.
- Addressing patient anxieties involves validating their feelings, providing reassurance, and answering their questions honestly and openly.
- Building trust involves demonstrating empathy, respect, and a commitment to the patient’s well-being.
Cultural Considerations: Addressing Diverse Needs
Cultural factors significantly influence help-seeking behaviors and access to mental health services. Providers must consider cultural beliefs, values, and communication styles when making referral decisions. A culturally sensitive approach ensures equitable access to care and promotes positive outcomes.
- Cultural barriers can include language differences, stigma surrounding mental illness, and mistrust of the healthcare system.
- A culturally sensitive approach involves using interpreters, providing culturally appropriate materials, and collaborating with community resources.
- Addressing diverse needs requires understanding and respecting cultural differences and adapting care to meet the specific needs of each patient.
Ultimately, referring a patient to urgent mental health services represents a critical intervention designed to protect lives and promote recovery. It’s a decision rooted in professional judgment, ethical responsibility, and a commitment to providing the best possible care. By understanding the multifaceted factors driving these referrals, we can better support both providers and patients navigating the complexities of mental health crises.
The collaborative efforts of providers, urgent care facilities, and support networks are crucial in ensuring a seamless transition to appropriate care and fostering positive outcomes.
Share this content:
