Medicare, Will It Pay for Phone Therapy?
Will medicare pay for o er telephone therapy mental health – Will Medicare pay for over-the-phone therapy for mental health? This question is increasingly important as telehealth expands. Many find the convenience of phone therapy appealing, but navigating Medicare coverage can be tricky. This guide clarifies Medicare’s current stance on telehealth mental health services, specifically those delivered via phone, outlining what’s covered, how to find participating providers, and the billing process.
We’ll also explore the advantages and disadvantages compared to in-person therapy and look at future trends in this rapidly evolving area of healthcare.
Understanding Medicare’s coverage is crucial for accessing affordable mental healthcare. This guide breaks down the complexities, providing practical advice and resources to help you make informed decisions about your mental well-being.
Medicare Coverage of Telehealth Mental Health Services
Understanding Medicare’s coverage of telehealth mental health services is crucial for both beneficiaries and providers. This section clarifies the guidelines, requirements, and processes involved in accessing and receiving reimbursement for these vital services.
Supporting young people’s mental wellbeing is crucial, especially in challenging circumstances. World Mental Health Day 2021 highlighted the struggles faced by Palestinian refugee youth, and you can read more about the initiatives helping them on this page: world mental health day 2021 palestine refugee youth helping …. Understanding these challenges informs effective interventions, which is why learning about working with children with mental health needs and behavioral problems is so vital for professionals and caregivers alike.
Early intervention and support can make a significant difference in a child’s life and future.
Medicare’s Telehealth Coverage Guidelines for Mental Health
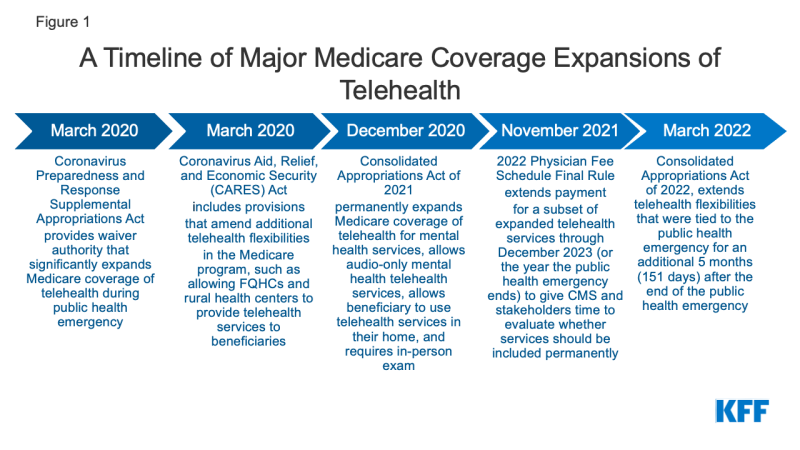
Medicare currently offers extensive coverage for telehealth mental health services. This coverage was significantly expanded during the COVID-19 pandemic and, in many cases, continues to be available even after the public health emergency ended. However, specific requirements and limitations apply, varying based on factors like the beneficiary’s location and the provider’s qualifications.
Supporting young people’s mental well-being is crucial, especially in challenging circumstances. World Mental Health Day 2021 highlighted the struggles faced by Palestinian refugee youth, and you can read more about the initiatives supporting them here: world mental health day 2021 palestine refugee youth helping …. This work underscores the importance of early intervention, which is why understanding how to working with children with mental health needs and behavioral problems is so vital for creating a supportive environment for their development and overall health.
Types of Mental Health Services Covered via Telehealth
A wide range of mental health services are typically covered by Medicare when delivered via telehealth. These include, but are not limited to, individual therapy sessions, group therapy, and psychiatric evaluations. Specific services and their coverage may vary depending on the individual’s Medicare plan and the provider’s participation status.
- Individual therapy sessions (e.g., Cognitive Behavioral Therapy, Dialectical Behavior Therapy)
- Group therapy sessions
- Psychiatric evaluations and medication management
- Substance abuse counseling
Provider Requirements for Medicare Reimbursement, Will medicare pay for o er telephone therapy mental health
To receive Medicare reimbursement for telehealth mental health services, providers must meet several requirements. These requirements ensure quality of care and compliance with Medicare regulations. Failure to meet these requirements can result in claim denials.
- Be enrolled in Medicare and participate in the Medicare telehealth program.
- Meet the state licensing requirements for their profession.
- Use a HIPAA-compliant platform for telehealth services.
- Comply with Medicare’s documentation and billing requirements.
- Provide services to beneficiaries in designated geographic areas (depending on the specific Medicare plan and coverage). In some cases, the patient must reside in a rural area or a designated Health Professional Shortage Area (HPSA).
Types of Telehealth Mental Health Services Covered
Medicare covers various telehealth modalities for mental health services, each with its own nuances regarding coverage and eligibility. Understanding these differences is essential for both patients and providers.
Specific Mental Health Conditions Covered

Medicare’s telehealth coverage extends to a broad spectrum of mental health conditions. This includes, but is not limited to, depression, anxiety, post-traumatic stress disorder (PTSD), schizophrenia, and bipolar disorder. The specific diagnosis does not usually affect the coverage itself, but rather the type and frequency of sessions recommended by the healthcare provider.
Telehealth Modalities and Medicare Coverage
Medicare typically covers both video conferencing and telephone therapy for mental health services. While video conferencing is generally preferred for its ability to facilitate a more comprehensive assessment and interaction, telephone therapy is also covered, particularly in situations where video conferencing is not feasible or accessible.
- Video Conferencing: Generally preferred, offering visual and auditory interaction.
- Telephone Calls: Acceptable in cases where video conferencing is unavailable or impractical.
Limitations on Session Duration and Frequency
While Medicare does cover telehealth mental health services, there might be limitations on the duration and frequency of sessions covered. These limitations often depend on the individual’s specific needs and the provider’s assessment. For example, some plans might have a cap on the total number of telehealth visits per year. It’s important to check with the specific Medicare plan for details.
Finding Medicare-Approved Providers
Locating mental health professionals who accept Medicare and offer telehealth services requires a strategic approach. Several resources and strategies can simplify this process.
Strategies for Locating Medicare-Approved Providers
Several resources can help individuals find Medicare-approved telehealth mental health providers. These resources can streamline the search and ensure the provider’s acceptance of Medicare and telehealth services.
- Medicare.gov: The official Medicare website offers a provider search tool.
- Physician finder tools: Many professional organizations maintain databases of healthcare providers.
- Referral networks: Primary care physicians or other healthcare providers can often provide referrals.
Verifying Provider Participation and Telehealth Capabilities
Once a potential provider is identified, verifying their Medicare participation and telehealth capabilities is essential. This verification ensures the provider is authorized to bill Medicare for telehealth services.
- Directly contact the provider’s office: Inquire about their Medicare participation status and telehealth services offered.
- Check the provider’s website: Many providers clearly state their Medicare participation and telehealth capabilities.
Medicare Reimbursement Procedures: Will Medicare Pay For O Er Telephone Therapy Mental Health
Understanding the billing and reimbursement procedures for telehealth mental health services under Medicare is crucial for both patients and providers. This section provides a step-by-step guide.
Billing and Reimbursement Procedures
The billing process for Medicare telehealth mental health services generally involves the provider submitting claims electronically to Medicare. The process can be quite detailed, with specific codes and documentation required. Providers use specific billing codes to indicate that the service was provided via telehealth.
Necessary Documentation for Reimbursement

Accurate and complete documentation is essential for successful reimbursement. This documentation must support the medical necessity of the services rendered.
- Patient’s demographic information
- Date and time of the telehealth visit
- Type of service provided
- Diagnosis codes
- Detailed notes of the session
Step-by-Step Guide for Patients
While patients are not directly involved in the billing process, understanding the basics can be helpful. The patient’s responsibility is typically to provide necessary information to the provider, such as their Medicare information.
Factors Affecting Medicare Coverage
Several factors can influence Medicare’s coverage of telehealth mental health services. Understanding these factors can help both patients and providers navigate the system effectively.
Geographic Location and Coverage
Geographic location plays a significant role in Medicare’s telehealth coverage. In some cases, the beneficiary must reside in a rural area or a designated HPSA to be eligible for telehealth services. These rules are constantly evolving, so staying informed about changes in your area is important.
Provider Specialty and Qualifications
The provider’s specialty and qualifications also influence Medicare reimbursement. Only licensed and qualified mental health professionals can bill Medicare for these services. The provider must be properly credentialed with Medicare to ensure that the claims are processed correctly.
Potential Challenges and Obstacles
Despite the expanding coverage, challenges remain in accessing Medicare-covered telehealth mental health services. These challenges may include technological barriers, lack of access to high-speed internet, or finding a provider who accepts Medicare and offers telehealth services in a patient’s area.
Comparison: In-Person vs. Telehealth
Comparing in-person and telehealth mental health services under Medicare highlights the advantages and disadvantages of each approach.
Costs and Benefits: In-Person vs. Telehealth
While the cost of telehealth and in-person visits can vary, telehealth often presents advantages in terms of convenience and accessibility. In-person visits may offer a more personal and potentially more comprehensive interaction, depending on the patient’s needs and the provider’s approach. The overall cost-effectiveness often depends on factors like travel time and expenses associated with in-person visits.
Advantages and Disadvantages: Patient and Provider Perspectives
From the patient’s perspective, telehealth offers increased convenience and accessibility, eliminating travel time and expenses. However, some patients may prefer the personal interaction of in-person visits. From the provider’s perspective, telehealth can expand their reach and serve a wider patient base, but it also requires additional technological expertise and infrastructure.
Accessibility, Convenience, and Cost-Effectiveness
Telehealth generally enhances accessibility and convenience, particularly for patients in rural areas or those with mobility limitations. The cost-effectiveness can vary depending on the specific circumstances, but telehealth often reduces travel expenses and time commitments, potentially making it more cost-effective in the long run for many patients.
Future Trends in Medicare Coverage
Predicting future trends in Medicare’s telehealth mental health coverage requires considering technological advancements and evolving healthcare practices.
Potential Changes and Expansions
It’s likely that Medicare will continue to expand its telehealth coverage for mental health services in response to growing demand and technological advancements. This expansion might include broader coverage of different modalities and increased reimbursement rates to incentivize providers’ participation.
Influence of Technological Advancements
Advancements in technology, such as virtual reality and artificial intelligence, could significantly impact future Medicare policies. These technologies may offer new ways to deliver mental health services and could influence coverage decisions.
Addressing the Growing Demand
To address the growing demand for telehealth mental health services, future Medicare policies might focus on increasing access to broadband internet in underserved areas, providing financial incentives for providers to offer telehealth services, and streamlining the billing and reimbursement processes.
Securing mental healthcare shouldn’t be a financial burden. While navigating Medicare’s telehealth coverage for phone therapy requires careful planning, it’s increasingly accessible. By understanding the requirements, finding the right provider, and following the proper billing procedures, you can utilize this convenient and potentially cost-effective option. Remember to always verify your provider’s participation and stay updated on evolving Medicare policies to ensure seamless access to the care you need.
Share this content:
