Will Single Payer Insurance Hurt Mental Healthcare?
Will single payer insurance put mental health out of business? It’s a question sparking intense debate. The current US mental healthcare system struggles with accessibility and affordability, leaving many without the care they need. Private insurance often limits coverage and drives up costs, creating a system where many providers struggle to stay afloat. A single-payer system promises universal coverage, but concerns exist about potential impacts on providers’ reimbursement and the range of services offered.
This discussion will explore the potential benefits and drawbacks of a single-payer system for mental healthcare, examining how it might affect both providers and patients. We’ll look at international examples, analyze potential challenges, and consider strategies to ensure a successful transition that prioritizes quality care and equitable access for all.
The Current State of Mental Healthcare Access in the US
Access to mental healthcare in the United States is marked by significant disparities and challenges. Affordability, availability of providers, and insurance coverage inconsistencies create substantial barriers for many individuals seeking care. This section will explore the current landscape, outlining the types of services available, their costs, and the role of private insurance in shaping access.
Current Mental Healthcare Access Challenges
The current system faces numerous hurdles. Affordability is a major concern, with many treatments costing hundreds or even thousands of dollars per session. Geographic location significantly impacts access, with rural areas often lacking sufficient providers. Insurance coverage varies widely, with some plans offering limited mental health benefits or imposing restrictive pre-authorization requirements. This often leads to undertreatment and delayed care, exacerbating existing mental health conditions.
Types and Costs of Mental Health Services
A range of mental health services are available, including therapy (individual, group, family), psychiatric medication management, hospitalization, and intensive outpatient programs. Costs vary drastically depending on the type of service, provider’s experience, and location. Therapy sessions can range from $100 to $300 per hour, while psychiatric medication management can add another significant cost. Hospitalization for mental health crises can be extremely expensive, often exceeding tens of thousands of dollars.
The Role of Private Insurance Companies
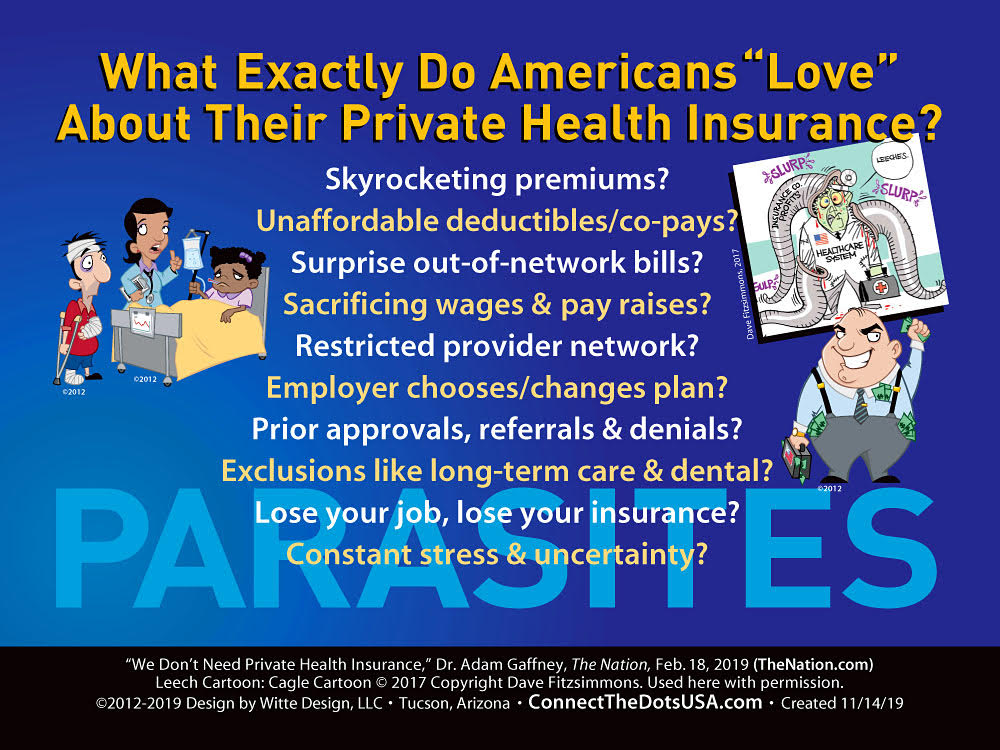
Private insurance companies play a substantial role in shaping access and affordability. Their decisions regarding coverage levels, reimbursement rates, and network restrictions directly impact patients’ ability to obtain care. Many plans impose limitations on the number of sessions covered, the types of providers included in their networks, and the specific treatments approved for reimbursement. This often forces individuals to choose between affordability and access to the most appropriate care.
Single-Payer System: Potential Impacts on Mental Healthcare
The implementation of a single-payer system for healthcare would significantly alter the landscape of mental healthcare provision. This section will analyze the potential effects on both providers and patients, considering the impact on reimbursement rates, provider participation, and patient access.
Impact on Mental Health Professionals’ Reimbursement Rates
A single-payer system would likely standardize reimbursement rates for mental health professionals. This could lead to either increased or decreased rates compared to the current system, depending on the specific design of the single-payer model. If rates are set too low, it could discourage providers from participating, potentially reducing access to care. Conversely, adequate reimbursement could attract more providers and enhance the quality of care.
Thinking about a career change? Remote work offers amazing flexibility, and if you’re a mental health professional, there are plenty of options. Check out these work from home mental health counselor jobs in Washington DC if you’re looking for a fulfilling role. It’s important to remember, though, that working too much can lead to mental health issues , so maintaining a healthy work-life balance is crucial, even in a remote setting.
Prioritizing self-care is key to preventing burnout and ensuring a sustainable career.
Potential Effects on Provider Participation
The number of mental health professionals willing to participate in a single-payer system is a critical factor. Lower reimbursement rates could drive some providers out of the system, especially those in private practice who rely heavily on higher fees from private insurance. However, a well-designed single-payer system with adequate reimbursement could incentivize greater participation, potentially attracting more providers to underserved areas.
Impact on Different Mental Health Provider Types
The impact of a single-payer system would likely vary across different mental health provider types. Psychiatrists, who often rely on medication management and have higher overhead costs, might be more sensitive to changes in reimbursement rates compared to therapists. Psychologists and social workers, who may have lower overhead, might be less affected. A single-payer system would need to account for these differences to ensure equitable access to a diverse range of mental healthcare services.
Single-Payer System: Potential Impacts on Patients
A single-payer system could dramatically reshape patients’ experiences with mental healthcare. This section will explore the potential impacts on access, coverage, and affordability from the patient perspective.
Impact on Patient Access to Mental Health Services
A single-payer system could improve access for many patients by eliminating the financial barriers to care. However, increased demand could lead to longer wait times for appointments, particularly for specialized services. The system’s design would be crucial in managing demand and ensuring timely access for all patients. Streamlined referral processes and expanded provider networks could mitigate potential wait time increases.
Impact on Types of Mental Health Services Covered, Will single payer insurance put mental health out of business
The range of mental health services covered under a single-payer system would depend on the specific design of the program. A comprehensive system would ideally cover a broad spectrum of services, including therapy, medication management, hospitalization, and specialized treatments. However, cost-containment measures might lead to limitations on certain services or the need for pre-authorization.
Impact on Affordability of Mental Health Services

For many patients, a single-payer system would significantly improve affordability. Eliminating out-of-pocket costs and co-pays would make mental healthcare accessible to individuals who currently cannot afford it. However, the system would need to be carefully designed to avoid compromising the quality of care in the name of cost reduction. Balancing cost-effectiveness and quality of care is crucial.
Comparison with Other Healthcare Systems
Examining mental healthcare systems in other countries with single-payer models provides valuable insights. This section will compare these systems to those with primarily private insurance models, highlighting key differences in access, affordability, and quality of care.
International Comparisons of Mental Healthcare Systems
Countries like Canada and the United Kingdom, with universal healthcare systems, generally demonstrate better access to mental healthcare compared to the US. While challenges exist in these systems (such as wait times), the financial barriers to care are significantly lower. In contrast, countries with primarily private insurance systems, such as the United States, often see greater disparities in access based on socioeconomic status and insurance coverage.
Access, Affordability, and Quality Differences
Single-payer systems typically offer greater access to mental healthcare services, particularly for low-income individuals. Affordability is significantly improved as patients face minimal or no out-of-pocket costs. Quality of care can vary, but generally, single-payer systems prioritize equitable access and strive for standardized quality measures. Private insurance models often lead to significant disparities in access and affordability, with quality varying depending on the specific insurance plan and provider.
Strengths and Weaknesses of Each Approach
Single-payer systems offer the advantage of universal access and improved affordability, promoting better mental health outcomes for the population. However, potential drawbacks include longer wait times and potential limitations on the range of services covered. Private insurance models can offer greater choice and potentially faster access for those with good insurance, but often lead to significant disparities in access and affordability.
Addressing Concerns about Mental Healthcare Under Single-Payer
Concerns exist regarding the potential impact of a single-payer system on mental healthcare access and quality. This section will explore strategies to mitigate these concerns and ensure a successful transition.
Strategies to Mitigate Concerns
To address concerns about reduced access, a single-payer system should prioritize expanding the mental health workforce, improving referral processes, and developing telehealth options to reach individuals in underserved areas. Investing in preventative mental health services can also reduce the overall demand for more intensive care.
Ensuring Adequate Reimbursement Rates
Adequate reimbursement rates for mental health professionals are crucial for attracting and retaining providers within a single-payer system. Regular reviews and adjustments of reimbursement rates, based on cost analyses and market trends, are necessary to ensure financial viability for providers. This should also consider the varying costs associated with different types of mental health professionals.
Maintaining a Diverse Range of Mental Health Services
Maintaining a diverse range of mental health services requires careful planning and resource allocation. The single-payer system should prioritize covering a broad spectrum of services, including specialized treatments, to meet the diverse needs of the population. Mechanisms for incorporating new and emerging treatments should also be in place.
The Role of Government Regulation
Government regulation plays a vital role in ensuring quality and access within a single-payer system. This section will explore the potential impact of different regulatory approaches.
Government Regulation and Quality Assurance
Government regulation can establish quality standards for mental healthcare services, including provider qualifications, treatment protocols, and data collection for performance monitoring. Regular audits and inspections can ensure adherence to these standards. This oversight helps maintain quality of care and protects patient safety.
Impact of Regulatory Approaches
Different regulatory approaches can significantly impact both providers and patients. Overly stringent regulations might stifle innovation and increase administrative burdens for providers. Conversely, insufficient regulation could compromise quality of care and patient safety. Finding a balance between effective oversight and avoiding excessive bureaucracy is critical.
Mechanisms for Monitoring and Improving Quality
Effective monitoring mechanisms are crucial for continuous improvement. These could include regular data collection on patient outcomes, provider performance, and system efficiency. Feedback mechanisms, such as patient surveys and provider input, can provide valuable insights for system adjustments and improvements. Regular reviews and revisions of regulations and policies based on data and feedback are also essential.
International Perspectives on Mental Health and Single-Payer Systems: Will Single Payer Insurance Put Mental Health Out Of Business
Learning from the experiences of other countries with single-payer systems is crucial for informing the design of a US system. This section will highlight international examples and lessons learned.
International Examples and Experiences
Many countries with universal healthcare systems have successfully integrated mental healthcare into their single-payer models. The UK’s National Health Service (NHS) and Canada’s provincial healthcare systems offer examples of comprehensive mental health services, though with varying degrees of success in addressing access and wait times. These systems offer valuable lessons on effective program design and implementation, as well as challenges encountered along the way.
Thinking about a career change? Many find that working from home offers a better work-life balance, which is crucial, as working too much can lead to mental health issues. If you’re a mental health counselor in the Washington DC area, consider the flexibility of remote work. There are actually quite a few work from home mental health counselor jobs Washington DC options available.
It could be the perfect way to help others while prioritizing your own well-being.
Comparison of Successes and Challenges
While single-payer systems often improve access and affordability, challenges such as wait times for specialized services and workforce shortages are common. Successfully integrating mental healthcare requires adequate funding, workforce development, and effective resource allocation. Learning from the successes and failures of other countries helps avoid pitfalls and maximize the benefits of a single-payer system.
Lessons Learned for a US Single-Payer System
Key lessons learned from international experiences include the importance of adequate funding, workforce development, and a focus on prevention and early intervention. Effective integration of mental healthcare requires a multi-faceted approach, encompassing service delivery models, provider training, and patient education. A phased implementation, starting with pilot programs and careful monitoring, can help ensure a smooth transition and address potential challenges proactively.
The transition to a single-payer system for mental healthcare presents both opportunities and challenges. While concerns about provider reimbursement and service availability are valid, they are not insurmountable. By learning from international experiences and implementing thoughtful strategies, including robust government regulation and proactive solutions to address potential shortfalls, we can strive towards a system that ensures accessible, affordable, and high-quality mental healthcare for everyone.
The ultimate goal is a system that prioritizes mental health alongside physical health, recognizing its crucial role in overall well-being.
Share this content:
