Mental Health Records, Progress Notes
With regard to progress notes in mental health records __________ – Mental Health Records: Progress Notes are crucial for effective patient care. This guide explores the legal, ethical, and practical aspects of documenting patient progress, from HIPAA compliance and best practices for note-writing to the impact of technology and cultural considerations. We’ll delve into how progress notes inform treatment planning, facilitate communication between healthcare providers, and ultimately contribute to improved patient outcomes.
We’ll cover essential components of a well-structured progress note, discuss strategies for overcoming common challenges like time constraints and maintaining objectivity, and examine how technological advancements like EHRs and telehealth are shaping the future of progress note documentation. The importance of cultural sensitivity in documenting patient information will also be addressed.
Progress Notes in Mental Health Records: A Comprehensive Guide: With Regard To Progress Notes In Mental Health Records __________
Progress notes are the cornerstone of comprehensive mental health care, serving as a vital record of patient encounters, treatment plans, and progress. They are crucial for ensuring continuity of care, facilitating effective communication among healthcare providers, and safeguarding patient well-being. This guide explores the legal, ethical, and practical aspects of progress note documentation in mental health settings.
HIPAA Regulations and Patient Privacy, With regard to progress notes in mental health records __________
The Health Insurance Portability and Accountability Act (HIPAA) establishes strict regulations to protect the privacy and security of Protected Health Information (PHI), including mental health records. HIPAA mandates that healthcare providers implement appropriate safeguards to prevent unauthorized access, use, or disclosure of PHI. This includes physical security measures, such as secure storage of paper records and access controls for electronic health records (EHRs), as well as administrative safeguards, such as implementing policies and procedures for handling PHI.
Violation of HIPAA regulations can result in significant civil and criminal penalties.
Ethical Considerations in Documentation
Documenting sensitive patient information necessitates a strong ethical foundation. Confidentiality is paramount, and providers must adhere to strict ethical guidelines to protect patient privacy. Informed consent is essential; patients must understand how their information will be used and have the right to access and amend their records. Ethical considerations also extend to the accuracy and objectivity of the documentation itself, ensuring that progress notes reflect the patient’s experience without bias or judgment.
Legal Ramifications of Inaccurate or Incomplete Notes
Inaccurate or incomplete progress notes can have serious legal ramifications. They can lead to misdiagnosis, inappropriate treatment, and potentially harm the patient. In legal proceedings, poorly documented records can be used against the provider, leading to malpractice lawsuits. Therefore, meticulous and accurate documentation is crucial to protect both the patient and the healthcare provider.
Best Practices for Writing Comprehensive Progress Notes
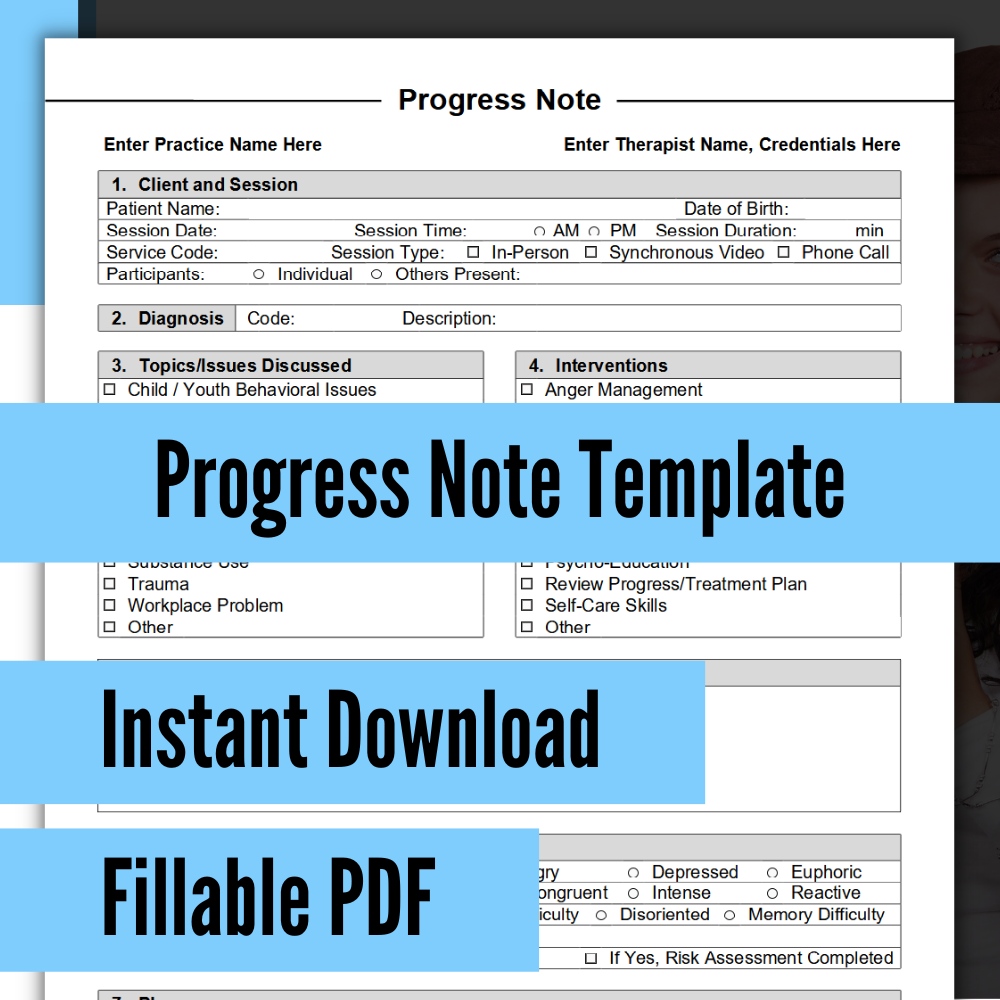
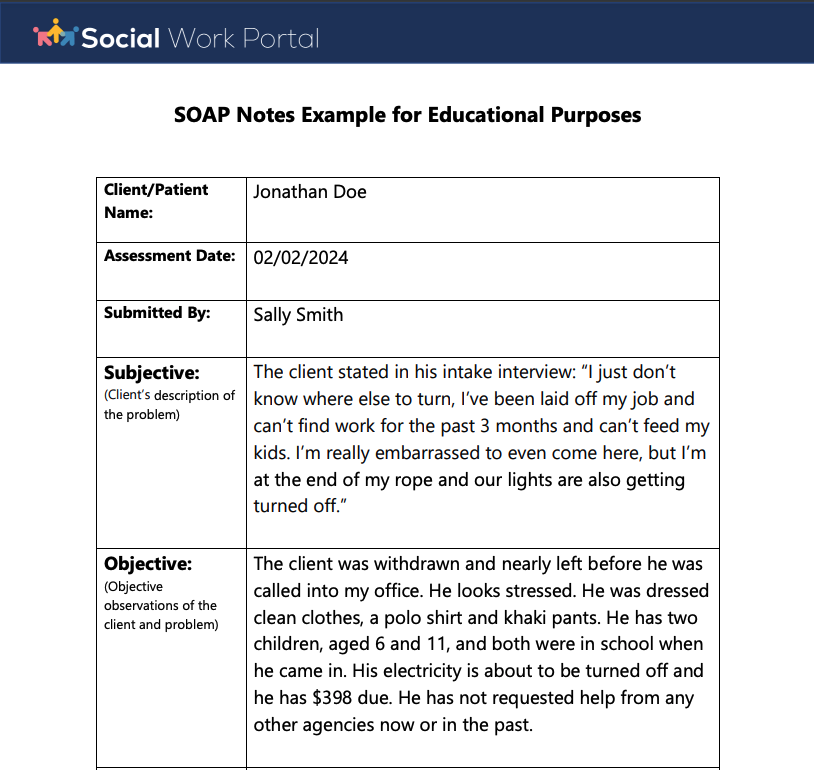
Effective progress notes should be clear, concise, and comprehensive. They should include a description of the presenting problem, a thorough assessment of the patient’s condition, a detailed treatment plan, and a record of progress toward goals. A standardized format can improve consistency and readability. For example, a SOAP note (Subjective, Objective, Assessment, Plan) format organizes information logically.
Mental health is a crucial aspect of overall well-being, and it’s great to see increasing awareness around it. For instance, the news about Y Williams reportedly taken to hospital for a mental health check highlights the importance of seeking help when needed. This brings to mind Robert Wubbolding’s work, as Wubbolding emphasizes that reality therapy is a mental health system , offering a structured approach to addressing these issues.
Early intervention and access to effective therapies are key to positive outcomes.
Other formats, like DAP (Data, Assessment, Plan) notes, are also commonly used. The choice depends on individual preferences and institutional requirements.
Sample Progress Note Format
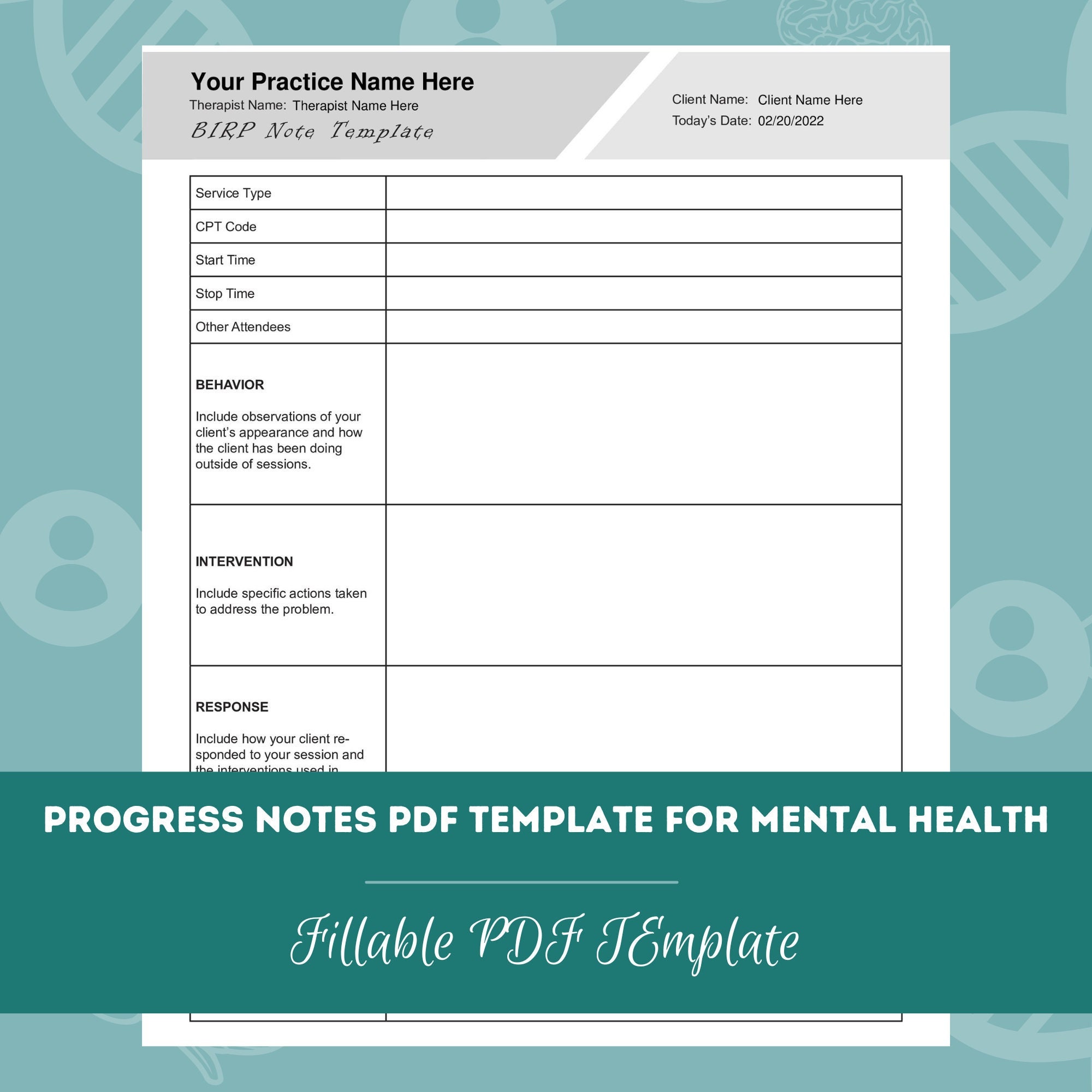
A sample progress note might include:
- Date: [Date of session]
- Patient Name: [Patient’s Name]
- Presenting Problem: [Brief description of the patient’s chief complaint]
- Assessment: [Observations and clinical findings]
- Plan: [Treatment plan and goals]
- Progress: [Progress made toward goals]
This format ensures that all key information is captured while maintaining brevity and clarity.
Progress Notes in Treatment Planning and Evaluation
Progress notes are integral to treatment planning and evaluation. They provide a detailed record of the patient’s journey, allowing for continuous monitoring and adjustment of the treatment plan. By tracking changes in symptoms, behaviors, and responses to interventions, clinicians can identify areas where adjustments are needed and make data-driven decisions to optimize patient outcomes. Significant changes or lack of progress as documented in the notes can signal the need for reassessment, modification of the treatment approach, or referral to other specialists.
Technological Advancements and Their Impact
Electronic Health Records (EHRs) have revolutionized progress note documentation, offering improved efficiency, accessibility, and data security. However, challenges remain, such as the potential for system errors and the need for robust training to ensure effective use. The emergence of AI-powered tools offers the potential to further streamline the documentation process and enhance accuracy by automating certain tasks. Telehealth and remote monitoring have altered the format and content of progress notes, requiring documentation of virtual interactions and remote monitoring data.
Challenges and Potential Solutions in Documentation
Common challenges include time constraints, ambiguity in terminology, and maintaining objectivity. To overcome these, efficient documentation techniques, such as using templates and standardized language, are crucial. Regular training and supervision can enhance consistency and accuracy. Employing clear and concise language reduces ambiguity, while self-reflection and peer review can help maintain objectivity. A structured approach to documentation, with regular review and updates, can improve overall quality and consistency.
Cultural Considerations in Progress Note Documentation
Cultural sensitivity is paramount in mental health documentation. Clinicians must avoid bias and stereotypes, recognizing that cultural factors can significantly influence the presentation and interpretation of mental health symptoms. A culturally informed lens is crucial for accurate assessment and treatment planning, ensuring that interventions are appropriate and effective for diverse patient populations. Ethical considerations include ensuring that documentation avoids perpetuating harmful stereotypes or misinterpretations.
It’s interesting to consider how different approaches to mental health intersect. For instance, the article on Wubbolding’s emphasis on reality therapy as a complete mental health system provides a structured framework, contrasting with the more immediate news about Y Williams reportedly being taken to hospital for a mental health check. These situations highlight the varied ways individuals navigate mental wellbeing, ranging from proactive therapeutic systems to crisis intervention.
Both aspects are crucial components of a comprehensive mental health landscape.
Impact of Progress Notes on Patient Outcomes and Communication
Well-documented progress notes are essential for effective communication among healthcare providers, facilitating continuity of care across different settings. Clear and concise notes ensure that all relevant information is readily available, minimizing the risk of miscommunication and improving the coordination of care. They foster collaboration among the treatment team, leading to improved patient outcomes and enhanced quality of care.
Effective progress note documentation in mental health is not merely a record-keeping exercise; it’s a cornerstone of quality patient care. By adhering to legal and ethical guidelines, employing best practices in writing, and embracing technological advancements, mental health professionals can ensure that progress notes accurately reflect patient journeys, facilitate effective communication, and ultimately contribute to positive treatment outcomes. Understanding the nuances of this process is key to providing the best possible care.
Share this content:
