Patients Get Paranoid, Which Mental Health Conditions?
With what mental health condition do patients get paranoid – Patients Get Paranoid: Which Mental Health Conditions? This question delves into the complex relationship between paranoia and various mental health conditions. Paranoia, characterized by persistent feelings of being watched, followed, or conspired against, isn’t a standalone diagnosis but a distressing symptom that can significantly impact daily life. Understanding which conditions frequently present with paranoia is crucial for accurate diagnosis and effective treatment.
Several mental illnesses are strongly associated with paranoia. Schizophrenia, for example, often involves persistent delusional beliefs, including paranoid delusions of persecution or grandeur. Delusional disorder, another condition, centers entirely around non-bizarre delusions, some of which are paranoid in nature. Bipolar disorder, with its fluctuating moods, can also trigger psychotic episodes featuring paranoia. Even severe depression and anxiety can manifest with heightened paranoia, while substance abuse can induce temporary psychotic states, including paranoid ideation.
The severity and presentation of paranoia vary across these conditions, highlighting the need for careful clinical assessment.
Understanding Paranoia
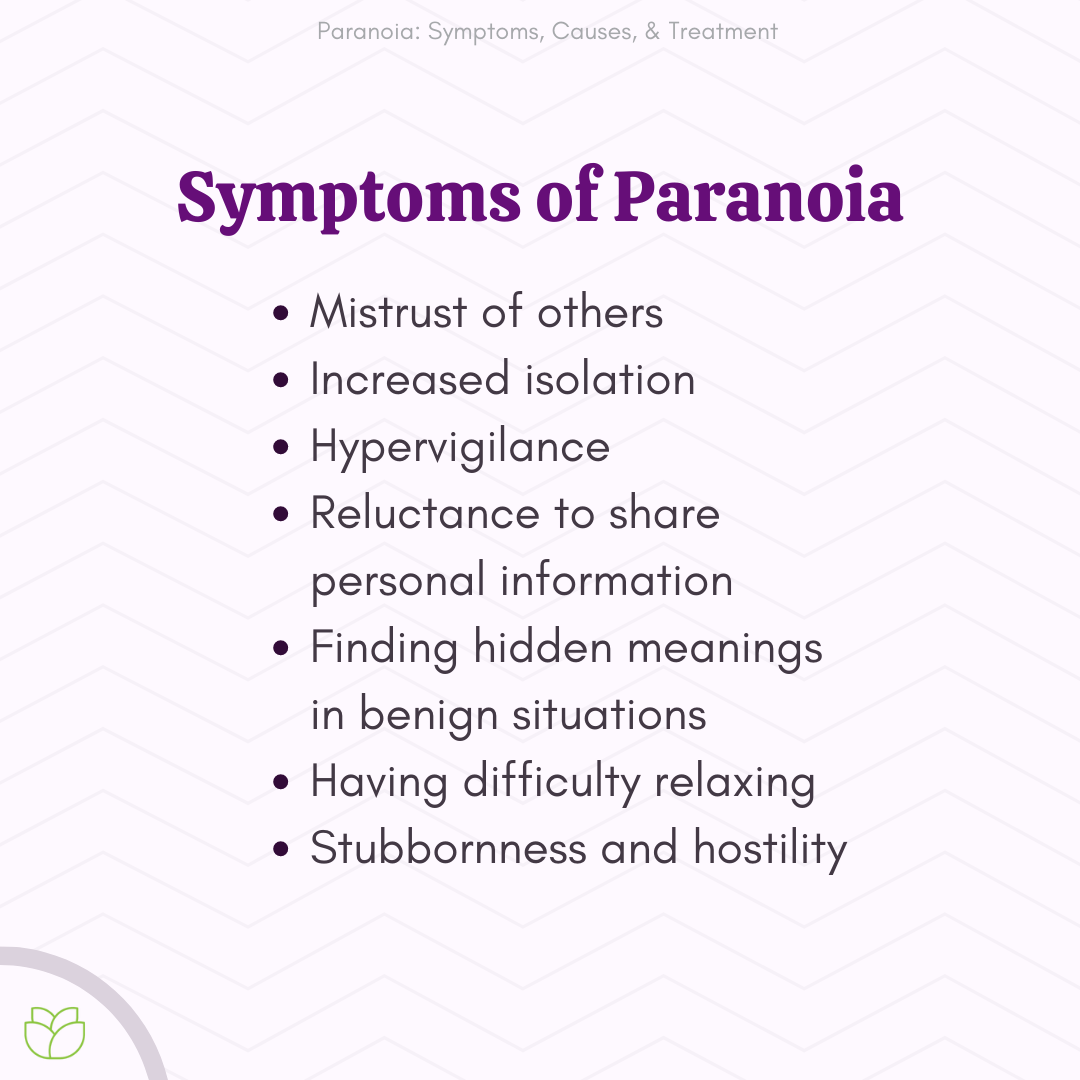
Paranoia, characterized by persistent, unfounded suspicions and distrust, significantly impacts an individual’s well-being. It’s crucial to understand that paranoia itself isn’t a standalone diagnosis but rather a prominent symptom present in various mental health conditions. Its manifestation varies widely, ranging from mild suspiciousness to deeply entrenched delusional beliefs that profoundly affect daily life and relationships.
Paranoia’s Manifestations and Impact
Paranoia can manifest in numerous ways. Individuals might experience intense feelings of being watched, followed, or conspired against. They may misinterpret others’ intentions, perceiving benign actions as threatening or malicious. This can lead to social isolation, strained relationships, and difficulty maintaining employment or education. The constant fear and suspicion associated with paranoia cause significant distress and impair daily functioning.
Mental Health Conditions and Paranoia
Several mental health conditions are strongly associated with paranoia. Understanding these connections is vital for accurate diagnosis and effective treatment.
Paranoia in Schizophrenia
Schizophrenia is a severe mental illness characterized by positive symptoms like hallucinations and delusions, including paranoid delusions. These delusions often involve beliefs of persecution, grandiosity, or control, significantly impacting a person’s perception of reality and their interactions with the world. For example, a person with schizophrenia experiencing paranoid delusions might believe that others are plotting against them or that they possess special powers.
Paranoia in Delusional Disorder
Delusional disorder, unlike schizophrenia, primarily involves non-bizarre, persistent delusions without other psychotic symptoms. Paranoid subtypes are common, with individuals holding fixed, false beliefs about being persecuted, cheated, or conspired against. The delusions are often more focused and systematized than in schizophrenia, lacking the broader range of symptoms. A person with delusional disorder might believe their spouse is having an affair despite overwhelming evidence to the contrary.
Paranoia in Bipolar Disorder
Bipolar disorder, marked by extreme mood swings between mania and depression, can involve psychotic symptoms, including paranoia, particularly during manic episodes. During these periods, individuals may experience grandiose delusions and heightened suspiciousness, leading to impulsive and erratic behavior. For instance, an individual in a manic state might believe they have exceptional abilities and become suspicious of those who question their claims.
Thinking about a career in pediatrics? The Woodhull Medical and Mental Health Center program pediatric residency might be a great fit. It’s demanding, of course, and the pressures of medical training can impact mental well-being, a concern highlighted in research on work organization and mental health problem in PhD students. This research underscores the importance of prioritizing mental health in demanding academic and professional settings, a lesson relevant across various fields, including medicine.
Comparing Paranoia in Schizophrenia and Delusional Disorder
While both conditions feature paranoia, schizophrenia presents with a broader range of psychotic symptoms, including hallucinations and disorganized thinking, whereas delusional disorder is primarily defined by the presence of persistent delusions without other significant psychotic symptoms. The intensity and pervasiveness of paranoia also differ, typically being more severe and disruptive in schizophrenia.
Paranoia in Severe Depression
Severe depression can sometimes manifest with psychotic features, including paranoid delusions. These delusions often center on themes of worthlessness, guilt, or impending doom. The presence of paranoia in depression complicates treatment, as it can interfere with engagement in therapy and medication adherence.
Paranoia and Anxiety Disorders
While not a core symptom, heightened paranoia can be a feature of some anxiety disorders. Individuals with severe anxiety may experience intense feelings of being watched or judged, leading to social avoidance and difficulty functioning in daily life. The constant worry and hypervigilance associated with anxiety can fuel paranoid thoughts.
Substance-Induced Psychotic Disorders
Substance use, particularly of stimulants like methamphetamine or cocaine, can induce psychotic symptoms, including paranoia. These substance-induced psychotic disorders often resolve upon cessation of substance use, but the experience can be highly distressing and potentially lead to long-term mental health challenges.
Prevalence of Paranoia Across Mental Health Conditions
The prevalence of paranoia varies significantly across different mental health conditions. It is highly prevalent in schizophrenia and delusional disorder, frequently present in bipolar disorder during psychotic episodes, and can occur in severe depression and anxiety disorders. Substance-induced psychotic disorders also commonly involve paranoia. Precise prevalence rates vary depending on the specific diagnostic criteria and population studied.
Biological and Psychological Factors in Paranoia
The development of paranoia involves a complex interplay of biological and psychological factors.
Neurobiological Mechanisms
Research suggests that imbalances in neurotransmitters, particularly dopamine, may contribute to paranoia. Structural and functional abnormalities in brain regions involved in processing social information and threat perception might also play a role. Specific neurobiological mechanisms vary depending on the underlying mental health condition.
Genetic Factors
Genetic predisposition significantly increases vulnerability to developing paranoia. Family history of schizophrenia, bipolar disorder, or other psychotic illnesses elevates the risk of experiencing paranoid symptoms. However, genetic factors alone do not determine the development of paranoia; environmental factors also play a crucial role.
Environmental Stressors
Trauma, abuse, neglect, and significant life stressors can trigger or exacerbate paranoid thoughts. These experiences can shape an individual’s perception of the world, making them more susceptible to developing paranoid beliefs. For example, a history of betrayal might lead to increased distrust and suspicion.
Cognitive Distortions
Cognitive distortions, such as confirmation bias (seeking information confirming existing beliefs while ignoring contradictory evidence) and jumping to conclusions, contribute to maintaining paranoid beliefs. Individuals may interpret ambiguous situations in a negative light, reinforcing their suspicions.
Thinking about a career in pediatrics? The Woodhull Medical and Mental Health Center program pediatric residency might be a great fit. It’s crucial to consider the pressures of medical training, though, and how they might impact well-being. This is especially relevant given the findings of research on work organization and mental health problem in PhD students , which highlights the importance of supportive work environments for mental health across various demanding fields.
A healthy work-life balance is essential, regardless of your chosen profession.
Maladaptive Coping Mechanisms
Maladaptive coping mechanisms, such as social isolation and avoidance, can inadvertently reinforce paranoid beliefs. By avoiding situations that might trigger anxiety or challenge their beliefs, individuals limit opportunities to test the validity of their suspicions.
Diagnostic Considerations and Differential Diagnosis
Accurately diagnosing the underlying cause of paranoia requires a comprehensive assessment.
Comprehensive Diagnostic Assessment
A thorough evaluation involves a detailed clinical interview, review of medical history, and potentially neuropsychological testing. Clinicians assess the presence and severity of various symptoms, including delusions, hallucinations, mood disturbances, and cognitive impairments, to differentiate between various mental health conditions.
Differentiating Paranoia as a Symptom and Primary Diagnosis
Distinguishing paranoia as a symptom from a primary diagnosis (like delusional disorder) requires careful consideration of the symptom’s context, duration, and association with other symptoms. The presence of additional psychotic symptoms, mood disturbances, or cognitive deficits helps determine the underlying condition.
Evaluation of Paranoid Symptoms
Clinicians use structured interviews and rating scales to evaluate the content, intensity, and impact of paranoid symptoms. Questions explore the nature of the delusions, the individual’s level of insight into their beliefs, and the degree to which the symptoms interfere with daily life. A thorough history of the onset and course of symptoms is also crucial.
Hypothetical Case Study
Consider a patient presenting with persistent beliefs of being followed and monitored. Determining whether this is delusional disorder, schizophrenia, or a symptom of another condition requires evaluating the presence of hallucinations, disorganized thinking, mood disturbances, and the impact on overall functioning. A detailed history, including any past trauma or substance use, is essential for a comprehensive diagnosis.
Treatment Approaches for Paranoia: With What Mental Health Condition Do Patients Get Paranoid
Treatment for paranoia depends on the underlying condition and often involves a combination of medication and therapy.
Pharmacological Treatments
Antipsychotic medications are commonly used to reduce the intensity of paranoid symptoms. These medications work by affecting neurotransmitter levels in the brain. Mood stabilizers may be used in conjunction with antipsychotics, particularly in cases of bipolar disorder or severe depression with psychotic features.
Psychotherapy, With what mental health condition do patients get paranoid
Cognitive Behavioral Therapy (CBT) is a highly effective psychotherapy for managing paranoia. CBT helps individuals identify and challenge their maladaptive thoughts and beliefs, develop more realistic interpretations of situations, and learn coping strategies to manage anxiety and distress. Other evidence-based therapies, such as Acceptance and Commitment Therapy (ACT), may also be beneficial.
Comparison of Treatment Modalities
The effectiveness of different treatment modalities varies depending on the individual and the underlying condition. Medication is often necessary to reduce the severity of psychotic symptoms, while psychotherapy helps individuals develop coping skills and improve their overall functioning. A combination of both approaches is usually most effective.
Holistic Treatment Approach
A holistic approach, integrating medication, therapy, and supportive social networks, is crucial for successful management of paranoia. Support groups and family education can play a significant role in improving adherence to treatment and promoting overall well-being.
Living with Paranoia: Coping Strategies and Support
Individuals experiencing paranoia can benefit from various coping strategies and support systems.
Coping Strategies
Techniques like mindfulness, relaxation exercises, and grounding techniques can help manage anxiety and reduce the intensity of paranoid thoughts. Practicing self-compassion and challenging negative thought patterns are also beneficial.
Social Support
Strong social support networks are essential. Connecting with supportive friends, family members, or support groups provides a sense of belonging and reduces feelings of isolation. Open communication and understanding from loved ones are crucial.
Self-Care
Prioritizing self-care, including regular exercise, healthy eating, sufficient sleep, and engaging in enjoyable activities, promotes overall well-being and reduces stress, which can exacerbate paranoid symptoms.
Resources and Support Groups
/what-is-paranoid-schizophrenia-4155331_final-fa6c66e4d61144079a2fa4897743ea39.png)
Numerous resources are available, including mental health professionals, support groups specifically for individuals experiencing paranoia or related conditions, and online communities offering peer support and information. These resources provide valuable guidance, understanding, and a sense of community.
In conclusion, paranoia is a multifaceted symptom appearing across a spectrum of mental health conditions. While it’s crucial to differentiate paranoia as a symptom from a primary diagnosis, understanding its association with conditions like schizophrenia, delusional disorder, and bipolar disorder is vital. Effective treatment requires a holistic approach, combining medication, psychotherapy, and strong support systems. By recognizing the various factors contributing to paranoia and utilizing available resources, individuals can navigate this challenging experience and work towards improved mental well-being.
Share this content:
