Withdrawal Isnt a Mental Health Feature
Withdrawal can’t be a feature of a mental health disorder—or can it? This statement, while seemingly straightforward, delves into the complex interplay between substance use disorders and mental health conditions. Understanding the nuances of withdrawal symptoms and how they can mimic or exacerbate existing mental health issues is crucial for accurate diagnosis and effective treatment. Misdiagnosis can have serious consequences, highlighting the importance of careful clinical assessment and a holistic approach to patient care.
It’s crucial to remember that seeking help for mental health is a sign of strength, not weakness. If you’re concerned about a veteran, resources are available; check out this helpful guide on what to do if you’re worried about a veteran who needs mental health services. Furthermore, openly discussing mental health is becoming increasingly common, and thankfully, the stigma is lessening.
In fact, yes you can talk about mental health at work , and creating a supportive environment is vital for everyone’s well-being. Prioritizing mental health benefits both individuals and the workplace.
The line between substance withdrawal and the symptoms of a mental health disorder can be blurry. Many symptoms overlap, leading to diagnostic challenges. This exploration examines the physiological and psychological mechanisms of withdrawal from various substances, comparing them to the symptoms of different mental health disorders. We’ll look at case studies illustrating the difficulties in differentiating between the two, the role of comorbidity, and the ethical considerations involved in accurate diagnosis and treatment.
Understanding Mental Health Disorders and Substance Withdrawal: Withdrawal Can’t Be A Feature Of A Mental Health Disorder
The statement “Withdrawal can’t be a feature of a mental health disorder” is inaccurate and requires a nuanced understanding of mental health disorders, substance use disorders, and their complex interplay. This article will explore the characteristics of mental health disorders, the nature of withdrawal, and how these two concepts frequently overlap, highlighting the crucial need for accurate diagnosis and appropriate treatment.
Defining Mental Health Disorders and Their Characteristics
Mental health disorders are conditions that affect a person’s thinking, feeling, or behavior. Diagnosis is complex, requiring a comprehensive assessment by a qualified professional. The Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) and the International Classification of Diseases, 11th revision (ICD-11) provide standardized criteria for diagnosis, considering symptom duration, severity, and impact on daily functioning.
Symptoms vary widely depending on the specific disorder, ranging from anxiety and depression to psychosis and personality disturbances. For example, major depressive disorder involves persistent sadness, loss of interest, and sleep disturbances, while schizophrenia involves hallucinations and delusions.
The Concept of Withdrawal and its Association with Substance Use Disorders

Substance withdrawal refers to the group of symptoms that occur when a person abruptly stops or reduces their intake of a substance they’re physically dependent on. This dependence involves physiological adaptations to the substance, leading to withdrawal symptoms when the substance is no longer present. These symptoms are driven by neurochemical imbalances in the brain. Withdrawal symptoms vary significantly across substances.
Alcohol withdrawal can manifest as tremors, seizures, and delirium tremens (DTs), a life-threatening condition. Opioid withdrawal involves intense cravings, muscle aches, and vomiting. Stimulant withdrawal often leads to fatigue, depression, and intense cravings.
The severity and duration of withdrawal depend on factors such as the type and amount of substance used, the duration of use, and individual factors like genetics and overall health. A prolonged history of heavy substance use typically results in more severe and prolonged withdrawal.
Differentiating Withdrawal from Mental Health Disorder Symptoms
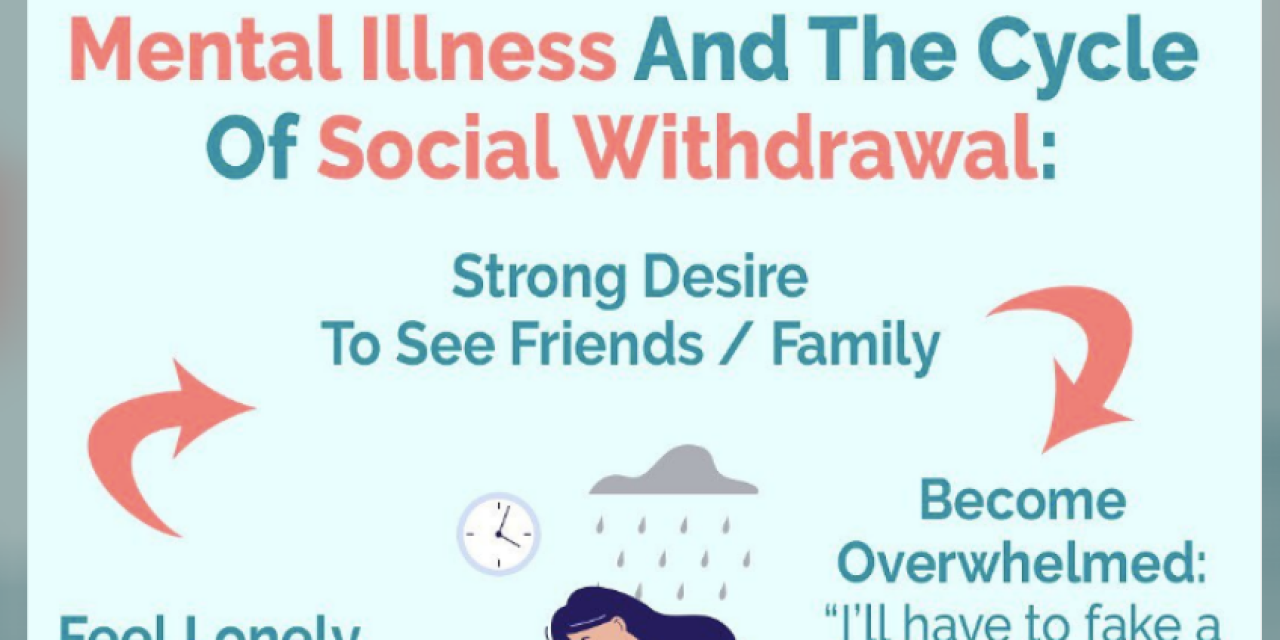
Differentiating withdrawal from mental health disorder symptoms can be challenging due to significant overlap. Anxiety, depression, irritability, and sleep disturbances are common to both withdrawal and various mental health disorders. Misdiagnosis can occur when withdrawal symptoms are mistaken for the primary disorder, or vice-versa. For instance, anxiety during opioid withdrawal might be misdiagnosed as an anxiety disorder, leading to inappropriate treatment.
Conversely, the depressive symptoms of a major depressive episode might be attributed solely to stimulant withdrawal, delaying necessary treatment for the underlying depression.
Consider a hypothetical case: a patient presents with intense anxiety, insomnia, and agitation. A history of heavy alcohol use is revealed. If the alcohol withdrawal is not recognized, the patient might be diagnosed with an anxiety disorder and treated accordingly, potentially leading to inadequate management of the withdrawal and its associated risks.
The Role of Comorbidity in Diagnoses
Comorbidity, the co-occurrence of mental health disorders and substance use disorders, is extremely common. Individuals with substance use disorders frequently experience other mental health conditions, and vice-versa. This co-occurrence significantly complicates diagnosis and treatment. The symptoms of both conditions can overlap and mask each other, making it difficult to determine which condition is primary and which is secondary.
Moreover, comorbidity can lead to poorer treatment outcomes if not addressed comprehensively.
Ethical Considerations in Diagnosis and Treatment
Misdiagnosing withdrawal as a mental health disorder has serious ethical implications. It can lead to inappropriate treatment, delaying necessary interventions to manage the withdrawal safely and effectively. Accurate diagnosis is crucial for developing effective treatment plans tailored to the individual’s specific needs. Healthcare professionals have a responsibility to conduct thorough assessments, considering all possible contributing factors, including substance use history and withdrawal symptoms, to avoid misdiagnosis and ensure appropriate care.
Treatment Approaches for Substance Use Disorders and Co-occurring Mental Health Disorders
Evidence-based treatment for substance use disorders typically involves a combination of approaches. Medication-assisted treatment (MAT) can help manage withdrawal symptoms and cravings. Psychotherapy, such as cognitive-behavioral therapy (CBT) and motivational interviewing, addresses underlying psychological factors contributing to substance use. Support groups, like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA), provide peer support and encouragement. Integrated treatment approaches are crucial when addressing comorbid conditions, ensuring that both the substance use disorder and the co-occurring mental health disorder are addressed simultaneously.
Addressing the Statement: “Withdrawal Can’t Be a Feature of a Mental Health Disorder”
The statement is fundamentally flawed. Withdrawal symptoms are frequently a significant component of the presentation and course of mental health disorders, especially in individuals with comorbid substance use disorders. The experience of withdrawal can exacerbate existing mental health conditions, or even trigger new ones. For example, alcohol withdrawal can induce severe anxiety and depression, worsening pre-existing anxiety or depressive disorders.
It’s crucial to remember that seeking help for mental health is a sign of strength, not weakness. If you’re worried about a veteran who needs mental health services, resources are available. Check out this helpful guide: worried about a veteran who needs mental health services. This support extends beyond veterans; it’s also important to know that yes you can talk about mental health at work , and creating a supportive work environment is key to fostering well-being for everyone.
The interaction between withdrawal and mental health conditions is complex and nuanced, requiring a holistic understanding to ensure effective diagnosis and treatment. The accurate assessment and management of withdrawal are essential for successful treatment of co-occurring mental health disorders.
Ultimately, the assertion that withdrawal cannot be a feature of a mental health disorder is an oversimplification. While withdrawal itself isn’t a mental health disorder, its symptoms significantly impact the presentation and course of co-occurring conditions. Accurate diagnosis requires a thorough understanding of both substance use disorders and mental health disorders, recognizing the potential for overlapping symptoms and the complexities of comorbidity.
A holistic approach that considers the individual’s entire clinical picture, including substance use history and current symptoms, is essential for effective treatment and improved patient outcomes.
Share this content:
