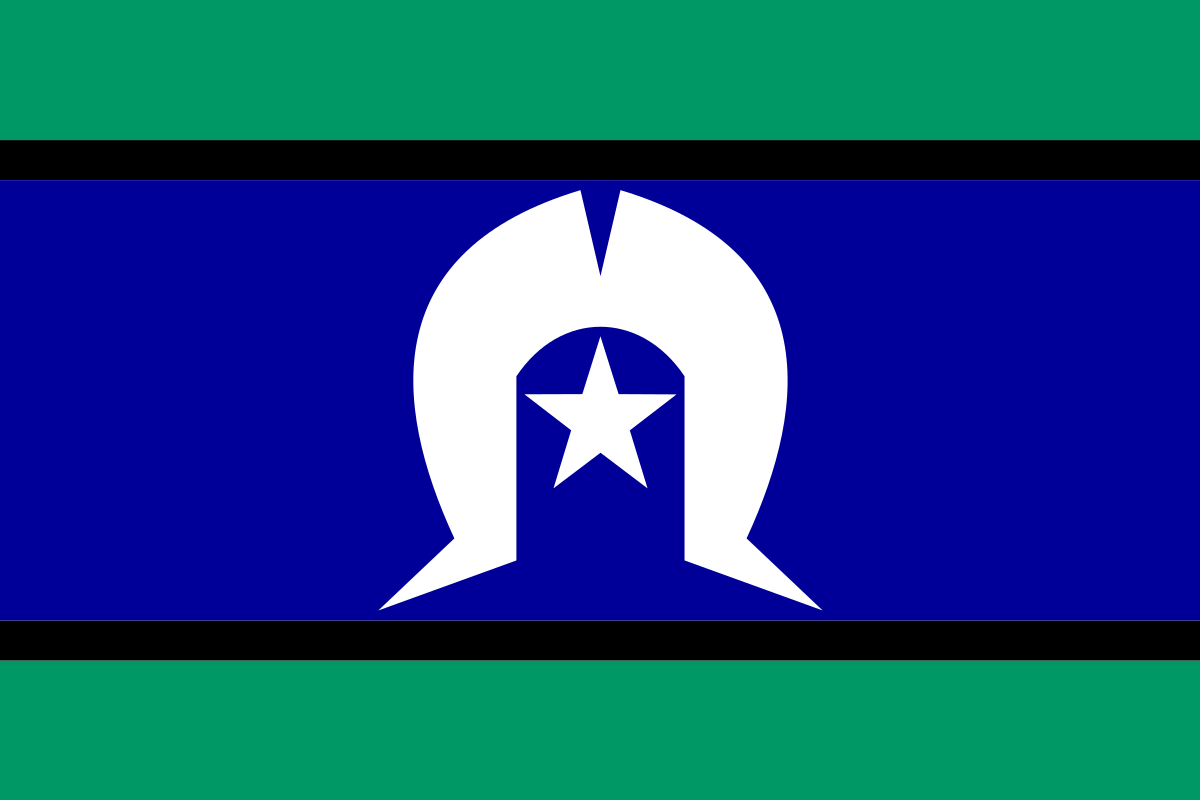
Working Together, Aboriginal & Torres Strait Islander Mental Health 2010
Working together aboriginal and torres strait islander mental health 2010 – Working Together: Aboriginal and Torres Strait Islander Mental Health 2010 offers a crucial snapshot of a critical period. This report examines the mental health landscape for Aboriginal and Torres Strait Islander peoples in 2010, exploring the challenges they faced, the existing support systems (or lack thereof), and the government initiatives in place. We’ll delve into the complexities of cultural safety, the impact of socioeconomic factors, and the vital role of community-based approaches.
The report analyzes both the successes and failures of government policies and community programs, highlighting the persistent barriers to accessing adequate mental healthcare. It also examines the limitations of available data and research at the time, emphasizing the need for culturally sensitive and evidence-based solutions. By understanding the past, we can better inform present and future strategies for improving mental health outcomes for this population.
Aboriginal and Torres Strait Islander Mental Health in 2010
The year 2010 presented a complex picture of mental health within Aboriginal and Torres Strait Islander communities. Significant disparities existed compared to the non-Indigenous population, stemming from a confluence of historical trauma, ongoing social disadvantage, and limited access to culturally appropriate care. This section will examine the prevalent challenges, contributing factors, and the state of mental health services available at that time.
The mental health landscape is constantly evolving, and understanding its intricacies is crucial. For researchers, the world journal of psychiatry and mental health research impact factor provides valuable insight into the field’s leading publications. This information is especially relevant considering the urgent need for improved workplace support, as highlighted by the recent article stating that workplaces should do more to support mental health expert says.
A strong emphasis on mental well-being in both research and the workplace is vital for a healthier future.
Mental Health Challenges in 2010
Aboriginal and Torres Strait Islander peoples in 2010 faced disproportionately high rates of mental health issues, including depression, anxiety, substance abuse, and self-harm. The impact of historical trauma, such as the Stolen Generations and ongoing systemic racism, significantly contributed to these elevated rates. Furthermore, the prevalence of chronic diseases and limited access to quality healthcare exacerbated existing mental health vulnerabilities.
Socio-Economic Factors Contributing to Disparities
Several socio-economic factors played a crucial role in the mental health disparities observed in 2010. These included high rates of poverty, unemployment, limited educational opportunities, inadequate housing, and exposure to violence and trauma within communities. The cumulative effect of these factors created a cycle of disadvantage, negatively impacting mental wellbeing.
Existing Mental Health Services and Accessibility
In 2010, mental health services for Aboriginal and Torres Strait Islander communities often lacked cultural sensitivity and accessibility. Geographical isolation, particularly in remote areas, presented a significant barrier to accessing care. Furthermore, a shortage of culturally competent mental health professionals and a lack of services delivered in Indigenous languages hindered effective service delivery.
Government Policies and Initiatives in 2010
The Australian government implemented various policies and initiatives in 2010 aimed at addressing the mental health needs of Aboriginal and Torres Strait Islander peoples. These initiatives varied in their approaches and effectiveness, reflecting the complexities of the issue.
The mental health landscape is constantly evolving, and understanding its complexities is crucial. A key metric for assessing the impact of research in this field is the impact factor, which you can check for the World Journal of Psychiatry and Mental Health Research here: world journal of psychiatry and mental health research impact factor. This data helps us understand the influence of published studies.
Meanwhile, the growing awareness of mental health in the workplace is vital, as highlighted by the recent article stating that workplaces should do more to support mental health, expert says. Both research and workplace support are key to improving overall well-being.
Key Government Policies and Initiatives
Examples of government initiatives included funding for culturally appropriate mental health programs, training programs for healthcare professionals on culturally safe practice, and initiatives to improve access to primary healthcare services in remote communities. Specific policy details and funding amounts would require referencing government documents from that period.
Effectiveness of Policies and Initiatives
Evaluating the effectiveness of these policies in 2010 is challenging due to limitations in data collection and analysis. While some programs showed promising results in improving access to care and promoting culturally safe practices, broader systemic changes were needed to address the underlying social determinants of mental health.
Comparison of Different Approaches
Government programs employed diverse approaches, ranging from community-based initiatives to top-down policy changes. Some focused on early intervention and prevention, while others prioritized treatment and rehabilitation. A comprehensive evaluation comparing the relative success of different approaches would require a detailed analysis of program evaluations from that era.
Community-Based Approaches and Programs in 2010
Community-based programs played a vital role in providing culturally safe and effective mental health services to Aboriginal and Torres Strait Islander communities in 2010. These programs often integrated traditional healing practices with Western approaches.
Examples of Successful Community-Based Programs

Many community-controlled health organizations delivered successful programs. These programs often incorporated traditional healing practices, such as storytelling, ceremonies, and connection to land and kinship, alongside Western mental health interventions. Specific examples would require referencing reports from individual organizations active at the time.
Principles of Culturally Safe and Appropriate Care
Culturally safe and appropriate care involved respecting Indigenous knowledge systems, involving community members in program design and delivery, and ensuring services were delivered in a way that was respectful of cultural protocols and beliefs. This often involved employing Indigenous health workers and utilizing local languages.
Role of Traditional Healing Practices, Working together aboriginal and torres strait islander mental health 2010
Traditional healing practices were often integral to community-based mental health programs. These practices provided culturally relevant and meaningful support, complementing Western approaches and fostering healing within a holistic framework. The integration of these practices varied across different communities and programs.
Challenges and Barriers to Accessing Care in 2010
Significant barriers hindered Aboriginal and Torres Strait Islander individuals from accessing adequate mental health services in 2010. These barriers were often interconnected and reinforced existing inequalities.
Key Barriers to Accessing Care
Key barriers included geographical remoteness, limited availability of culturally appropriate services, lack of transport, financial constraints, and systemic discrimination within the healthcare system. These factors created significant challenges for individuals seeking help.
Impact of Geographical Isolation, Cultural Differences, and Systemic Discrimination
Geographical isolation made accessing services difficult, especially in remote areas. Cultural differences between service providers and clients often led to misunderstandings and mistrust. Systemic discrimination resulted in unequal access to services and poorer quality of care.
Contribution of Barriers to Poorer Mental Health Outcomes
These barriers contributed to delayed or absent treatment, leading to poorer mental health outcomes, increased hospitalizations, and higher rates of suicide. Addressing these barriers was crucial for improving the mental wellbeing of Aboriginal and Torres Strait Islander peoples.
Future Directions and Recommendations (2010 Perspective)
Based on the situation in 2010, several recommendations emerged to improve mental health services and support for Aboriginal and Torres Strait Islander peoples. These recommendations prioritized culturally safe and effective care and addressed the identified barriers.
Recommendations for Improving Mental Health Services
- Increased funding for culturally appropriate mental health programs.
- Training of healthcare professionals in culturally safe practices.
- Improved access to primary healthcare services in remote areas.
- Development of culturally appropriate mental health resources and materials.
- Increased employment of Aboriginal and Torres Strait Islander health workers.
Strategies to Address Barriers and Promote Culturally Safe Care
Strategies included investing in telehealth technologies to overcome geographical barriers, implementing culturally sensitive training programs for all healthcare professionals, and addressing systemic discrimination within the healthcare system through policy changes and increased accountability.
Prioritized List of Recommendations
Prioritization of recommendations would depend on the specific context and available resources. However, addressing immediate access issues in remote communities and investing in culturally appropriate training for healthcare providers would likely be considered high priorities.
Cultural Considerations and Safe Practices in 2010
Cultural safety and appropriateness were paramount in providing effective mental health services to Aboriginal and Torres Strait Islander people in 2010. Ignoring cultural factors could severely compromise the quality of care and lead to mistrust and further harm.
Importance of Cultural Safety and Appropriateness
Cultural safety means ensuring services are delivered in a way that respects Indigenous knowledge, practices, and beliefs. This includes employing Indigenous health workers, providing services in Indigenous languages, and incorporating traditional healing practices into mainstream care.
Significance of Incorporating Indigenous Knowledge and Perspectives
Incorporating Indigenous knowledge and perspectives was crucial for developing effective and culturally relevant mental health interventions. This involved understanding the historical context of mental health issues within Aboriginal and Torres Strait Islander communities and recognizing the importance of kinship, community, and spirituality in healing.
Characteristics of a Culturally Safe Mental Health Service
A culturally safe mental health service would be characterized by a strong emphasis on self-determination, community participation, cultural sensitivity, respect for traditional healing practices, and the active involvement of Indigenous health workers in all aspects of service delivery.
Data and Research Limitations in 2010: Working Together Aboriginal And Torres Strait Islander Mental Health 2010

Data and research on Aboriginal and Torres Strait Islander mental health in 2010 faced several limitations, impacting the understanding of the issues and the development of effective interventions.
Limitations of Available Data and Research
Data collection methods often lacked cultural sensitivity, leading to underreporting and inaccurate representation of mental health issues within this population. Access to data was also limited, hindering comprehensive analysis and research.
Potential Biases in Existing Data
Existing data may have reflected biases in data collection methods, leading to an incomplete picture of the complexities of mental health within Aboriginal and Torres Strait Islander communities. For example, reliance on Western diagnostic frameworks might not accurately capture the nuances of mental distress experienced within Indigenous cultures.
Need for Further Research
Further research was needed to address the significant knowledge gaps, using culturally appropriate methods and involving Indigenous communities in the research process. This would enable a more accurate understanding of the challenges and inform the development of effective and culturally sensitive interventions.
Ultimately, “Working Together: Aboriginal and Torres Strait Islander Mental Health 2010” underscores the urgent need for culturally appropriate and accessible mental health services for Indigenous Australians. The report highlights the importance of collaboration between government, community organizations, and traditional healers to address systemic inequities and improve mental health outcomes. While the report focuses on 2010, its findings remain relevant today, reminding us of the ongoing need for sustained commitment and investment in culturally safe and effective mental health care for Aboriginal and Torres Strait Islander peoples.
Share this content:
