Why Mental Health Professionals Face High Complaint Risk
Wwhy mental health professional are at high risk for complaints – Why mental health professionals are at high risk for complaints is a crucial question demanding exploration. The demanding nature of the profession, coupled with complex ethical considerations and systemic pressures, creates a perfect storm for misunderstandings and complaints. This article delves into the multifaceted reasons behind this concerning trend, examining the contributing factors and offering potential solutions.
From the intense emotional toll of vicarious trauma and heavy caseloads to the intricate web of legal and regulatory frameworks, the challenges faced by mental health professionals are significant. Understanding these challenges is vital not only for protecting professionals but also for ensuring the quality and accessibility of mental health care.
The High Risk of Complaints Against Mental Health Professionals: Wwhy Mental Health Professional Are At High Risk For Complaints
Mental health professionals, despite their dedication to helping others, face a significant risk of complaints. This risk stems from a complex interplay of factors, including the inherent stressors of the profession, ethical dilemmas, legal complexities, and the expectations and perceptions of clients. Understanding these contributing factors is crucial for developing strategies to mitigate risk and improve the well-being of mental health professionals.
Prevalence of Complaints Against Mental Health Professionals, Wwhy mental health professional are at high risk for complaints
Complaints against mental health professionals are a considerable concern. While precise statistics vary depending on the country and reporting mechanisms, studies consistently show a noticeable rate of complaints. The types of complaints most frequently reported include boundary violations (e.g., dual relationships, inappropriate self-disclosure), negligence (e.g., failure to provide adequate care, misdiagnosis), and ethical breaches (e.g., confidentiality violations, conflicts of interest).
Demographic trends suggest that complaints may be more frequently filed against professionals with a longer career span, possibly reflecting accumulated stressors or a higher likelihood of encountering complex cases. Further research is needed to refine these demographic trends and their correlation with specific types of complaints.
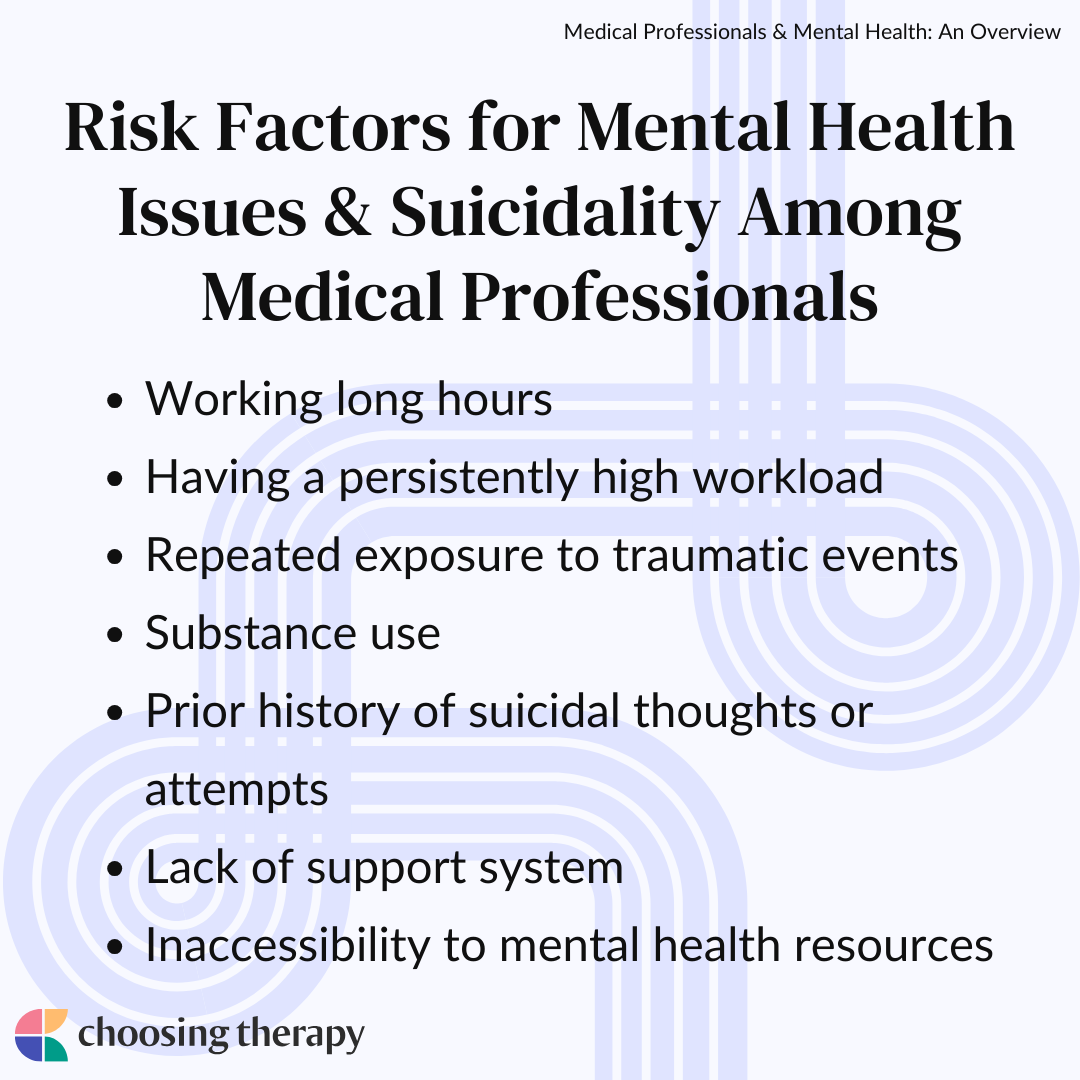
Stress and Burnout in the Mental Health Profession
The mental health profession is inherently demanding. Professionals frequently encounter distressing situations, including exposure to trauma narratives (vicarious trauma), managing heavy caseloads, navigating complex bureaucratic systems, and dealing with the emotional weight of their clients’ struggles. These factors significantly contribute to high levels of stress and burnout. Burnout manifests in various ways, such as emotional exhaustion, depersonalization, and a reduced sense of personal accomplishment.
This can lead to impaired professional judgment, decreased empathy, and increased risk of errors, ultimately increasing the likelihood of complaints. For example, a therapist experiencing severe burnout might struggle to maintain appropriate boundaries or provide effective treatment, leading to client dissatisfaction and potential complaints.
Ethical Dilemmas and Boundary Issues
Ethical dilemmas are commonplace in mental health practice. Situations involving conflicts of interest, confidentiality breaches, or the need to balance client autonomy with the professional’s responsibility to protect others can create significant challenges. Boundary issues, especially in the context of therapeutic relationships, are particularly sensitive. Even seemingly minor transgressions, such as accepting gifts from clients or engaging in social media interactions, can be misinterpreted and lead to complaints.
Maintaining clear professional boundaries, including establishing and adhering to clear guidelines for communication and interaction outside of therapy sessions, is essential to mitigating this risk. Regular supervision and self-reflection can help professionals navigate these complex situations effectively.
The Impact of Legal and Regulatory Frameworks
Mental health professionals operate within a complex web of legal and regulatory frameworks. Malpractice insurance and licensing requirements are essential for protecting both professionals and clients. However, these frameworks also contribute to the risk of complaints. The investigation and resolution of complaints can be lengthy and stressful, involving legal proceedings, disciplinary actions, and potential reputational damage. Understanding the specific legal and ethical obligations within one’s jurisdiction is paramount in minimizing risk.
The Role of Supervision and Peer Support
Adequate supervision and peer support are crucial for mitigating the risks faced by mental health professionals. Effective supervision provides a safe space for professionals to process challenging cases, explore ethical dilemmas, and receive guidance on best practices. Peer support networks offer a sense of community and shared experience, fostering resilience and reducing feelings of isolation. These networks provide opportunities for professionals to learn from each other, share coping strategies, and gain support during difficult times.
Hey, so I saw this awesome hoodie online, the ” you are bad for my mental health hoodie nihachu ” – it’s pretty funny, right? It got me thinking about mental health resources, though. Reading about the recent situation at Yale, specifically the article ” yale mental health held hospital new haven yale daily news “, highlighted the importance of accessible and quality mental healthcare.
It’s a serious issue, and it’s good to see discussions around improving access and support.
Regular participation in these supportive structures significantly reduces the likelihood of burnout and associated risks.
Improving Professional Practice and Reducing Risk

Minimizing the risk of complaints requires a multi-pronged approach. Best practices include maintaining meticulous documentation, engaging in regular self-reflection, seeking supervision, and participating in continuing education to stay updated on ethical guidelines and best practices. A framework for self-reflection might involve regular journaling, peer consultation, and seeking feedback from supervisors. Professional training should emphasize ethical decision-making, boundary setting, and strategies for managing stress and burnout.
So, I saw this hilarious hoodie online – the “You are bad for my mental health hoodie Nihachu” you are bad for my mental health hoodie nihachu – and it totally cracked me up. It’s a relatable statement for anyone who’s ever had a complicated relationship with their favorite streamer. Speaking of serious issues, I also read a concerning article about the Yale mental health situation, specifically yale mental health held hospital new haven yale daily news , highlighting the struggles students face accessing adequate care.
It’s a stark contrast to the lightheartedness of the hoodie, but both underscore the importance of mental well-being.
Client Expectations and Perceptions
Client expectations and perceptions of treatment significantly influence the likelihood of complaints. Clear communication and informed consent are essential for managing expectations and fostering a collaborative therapeutic relationship. Addressing client dissatisfaction promptly and constructively is also vital. Open communication channels, active listening, and a willingness to address concerns can prevent minor issues from escalating into formal complaints.
The Impact of the Mental Health System
Systemic factors within the mental health system also contribute to the risk of complaints. Resource limitations, bureaucratic processes, and inadequate support for professionals can create significant stressors. Improving the overall mental health system by providing adequate resources, streamlining bureaucratic processes, and offering robust support systems for professionals can reduce the risk of complaints and enhance the quality of care provided to clients.
Ultimately, addressing the high risk of complaints against mental health professionals requires a multi-pronged approach. This involves improving professional training, fostering supportive work environments, strengthening regulatory frameworks, and enhancing communication between professionals and clients. By proactively addressing these issues, we can create a more sustainable and supportive system for both professionals and those seeking their care, leading to better mental health outcomes for all.
Share this content:
