x-n Early Mental Health Intervention for First Responders
X-n early mental health intervention for first responders is crucial. First responders, the brave individuals who rush towards danger, often face unseen battles with mental health issues like PTSD, depression, and anxiety. The high-stress nature of their jobs, coupled with exposure to traumatic events, significantly impacts their well-being. This exploration delves into the challenges, effective intervention strategies, and the importance of fostering a supportive environment to protect these vital members of our communities.
Understanding the unique pressures faced by police officers, firefighters, paramedics, and other first responders is the first step. We’ll examine contributing factors, such as prolonged exposure to trauma, irregular work schedules, and the inherent risks of their professions. By analyzing the prevalence of mental health conditions within this population, we can develop targeted and effective intervention programs.
The Prevalence of Mental Health Issues Among First Responders
First responders, including police officers, firefighters, paramedics, and emergency medical technicians, face significantly higher rates of mental health issues compared to the general population. This is largely due to the unique and demanding nature of their jobs, exposing them to constant stress, trauma, and irregular work schedules. Understanding the specific challenges and contributing factors is crucial for developing effective early intervention strategies.
Mental Health Challenges Faced by First Responders
First responders frequently encounter traumatic events, witnessing death, injury, and suffering. This exposure can lead to a range of mental health problems, including post-traumatic stress disorder (PTSD), depression, anxiety, and substance abuse. Police officers, for example, may experience moral injury from having to make difficult decisions in high-pressure situations. Firefighters might grapple with the emotional toll of witnessing devastating fires and rescuing victims.
Paramedics regularly encounter critical injuries and illnesses, facing the potential for failure and loss. The cumulative effect of these experiences can be devastating.
Contributing Factors to High Rates of Mental Health Issues
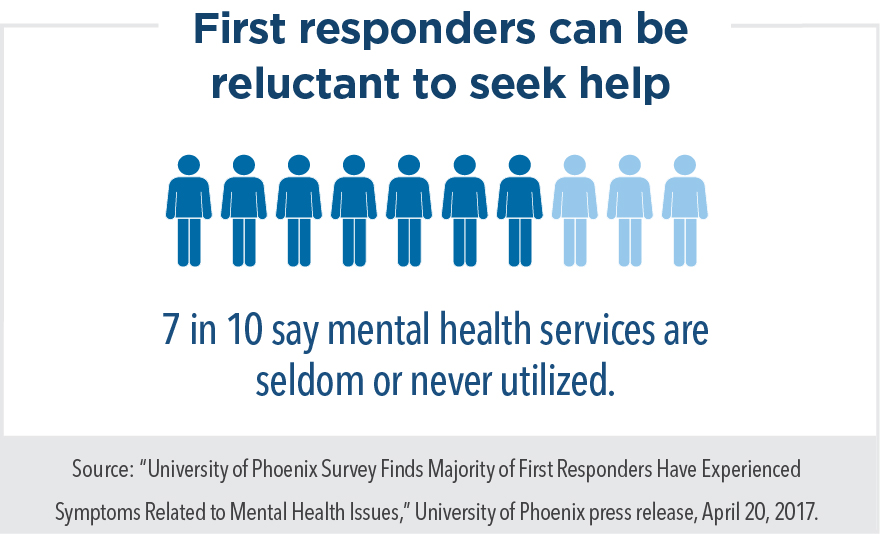
Several factors contribute to the elevated mental health challenges among first responders. Exposure to traumatic events is a primary driver, leading to PTSD and other trauma-related disorders. The high-stress work environment, characterized by long hours, unpredictable shifts, and life-or-death situations, adds to the pressure. Irregular work schedules disrupt sleep patterns and family life, further exacerbating stress. Limited social support, coupled with a culture that often discourages help-seeking, creates additional barriers to accessing care.
Furthermore, the inherent risks associated with their jobs, such as physical injury and exposure to hazardous materials, can significantly impact their well-being.
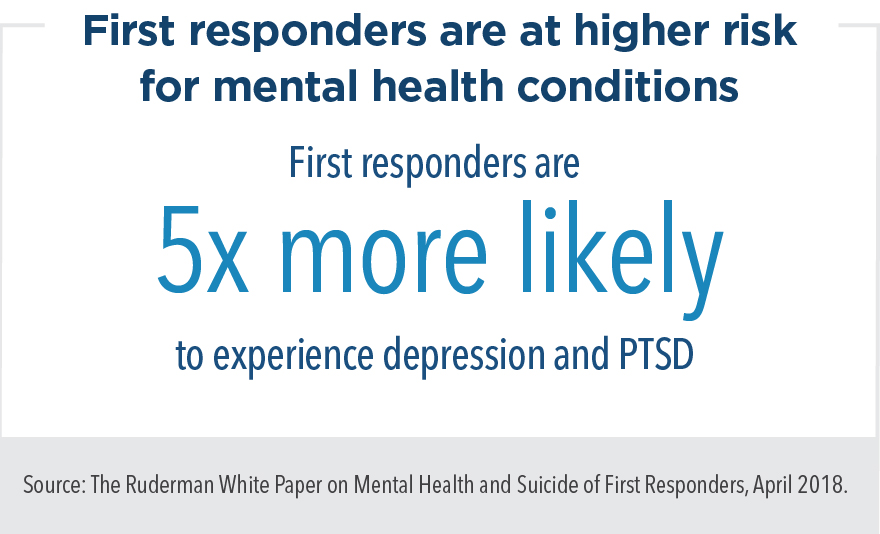
Statistics on Mental Health Issues Among First Responders
Studies consistently demonstrate high rates of mental health problems among first responders. While precise figures vary depending on the study and population, a significant percentage experience PTSD, depression, anxiety, and substance abuse at rates far exceeding the general population. For instance, studies have shown PTSD prevalence rates among police officers ranging from 10% to 30%, with similar elevated rates reported for firefighters and paramedics.
Similarly, depression and anxiety are significantly more prevalent among this population, often leading to substance abuse as a coping mechanism. These statistics underscore the urgent need for comprehensive mental health support programs specifically designed for this high-risk group.
Early Intervention Strategies: Identifying At-Risk Individuals
Early identification of at-risk first responders is critical in preventing the development of serious mental health conditions. A proactive approach, incorporating regular screening, wellness evaluations, and open communication, is essential for fostering a supportive environment where help-seeking is encouraged.
Screening Process for Identifying At-Risk First Responders
A multi-faceted screening process should be implemented. This could involve periodic anonymous surveys assessing symptoms of PTSD, depression, anxiety, and substance abuse. Regular wellness evaluations, conducted by trained professionals, can provide a more comprehensive assessment. Supervisors should also be trained to recognize signs of distress and encourage their team members to seek help. Furthermore, confidential peer support programs can play a vital role in early identification and intervention.
Proactive Mental Health Checks and Wellness Evaluations
Regular mental health checks should be incorporated into routine health assessments. These checks could involve brief questionnaires, interviews, or more comprehensive psychological evaluations, depending on the individual’s needs and risk factors. Wellness evaluations should go beyond mental health, addressing physical health, stress management, and work-life balance. The goal is to create a culture of proactive self-care and encourage early intervention before problems escalate.
Fostering Open Communication and Reducing Stigma
Creating a culture of open communication is crucial. This involves leadership actively promoting mental health awareness, reducing the stigma associated with seeking help, and ensuring that help-seeking is viewed as a sign of strength, not weakness. Educational programs, workshops, and peer support groups can help destigmatize mental health issues and encourage open dialogue within the first responder community.
Types of Early Mental Health Interventions
A range of interventions can effectively address the mental health needs of first responders. These interventions should be tailored to the individual’s specific needs and preferences, considering the nature and severity of their mental health challenges.
Various Intervention Methods for First Responders
- Therapy: Cognitive Behavioral Therapy (CBT) and trauma-focused therapies, such as prolonged exposure therapy (PE) and eye movement desensitization and reprocessing (EMDR), are highly effective in treating PTSD, anxiety, and depression.
- Peer Support Programs: Connecting first responders with trained peers who understand their experiences can provide invaluable support, reduce isolation, and encourage help-seeking.
- Mindfulness Techniques: Mindfulness-based stress reduction (MBSR) and other mindfulness practices can help manage stress, improve emotional regulation, and enhance overall well-being.
- Medication Management: In some cases, medication may be necessary to manage symptoms of depression, anxiety, or PTSD. This should be determined by a qualified healthcare professional.
Effectiveness of Different Interventions
The effectiveness of different interventions varies depending on the specific mental health condition and individual factors. For example, CBT is generally effective for anxiety and depression, while trauma-focused therapies are often preferred for PTSD. A combination of approaches, such as therapy combined with peer support or mindfulness techniques, may be most beneficial for many individuals. Regular evaluation and adjustment of the intervention plan are essential to ensure its effectiveness.
Resources Available to First Responders, X-n early mental health intervention for first responders
Many resources are available to first responders seeking mental health support. These include employee assistance programs (EAPs), specialized mental health clinics, and peer support networks. National organizations dedicated to first responder mental health often provide valuable resources and information. It’s crucial that first responders are aware of and have easy access to these resources.
The Role of Leadership and Organizational Support

Organizational leadership plays a pivotal role in creating a supportive environment that encourages help-seeking and promotes the mental well-being of first responders. This requires a commitment to implementing effective mental health policies and programs, coupled with fostering a culture of understanding and support.
Responsibility of Supervisors and Organizational Leaders
Supervisors and leaders have a responsibility to model healthy behaviors, actively promote mental health awareness, and create a culture of open communication. They should be trained to recognize signs of distress in their team members and encourage them to seek help. Furthermore, they should ensure that mental health resources are readily available and accessible to all members of the organization.
Implementing Effective Mental Health Policies and Programs
Effective mental health policies should include provisions for confidential access to mental health services, paid time off for mental health treatment, and reasonable accommodations for individuals with mental health conditions. Comprehensive mental health programs should offer a range of services, including screening, therapy, peer support, and wellness initiatives.
Creating a Supportive Work Environment
A supportive work environment is characterized by open communication, mutual respect, and a culture that values mental well-being. This involves creating opportunities for team building, fostering camaraderie, and promoting a sense of belonging. Leaders should actively address stigma and ensure that seeking mental health support is not viewed negatively.
The Importance of Family and Community Support
Family and community support systems play a crucial role in the recovery process of first responders. The stress and trauma experienced on the job can significantly impact family relationships, and strong support networks are essential for mitigating these impacts and promoting resilience.
Role of Family Members in Recovery
Family members can provide emotional support, practical assistance, and encouragement during challenging times. Understanding the unique challenges faced by first responders is crucial for family members to provide effective support. Open communication, empathy, and patience are essential for fostering a supportive family environment.
Community Support for First Responders
Community support can take many forms, including peer support groups, community events, and local organizations offering mental health services. Community involvement can provide a sense of belonging and reduce isolation, while access to local resources can facilitate timely access to needed care.
Strategies for Family and Community Support
Families and communities can support first responders by educating themselves about PTSD, depression, and other mental health conditions. They can also offer practical assistance, such as childcare or household chores, to alleviate stress. Creating opportunities for social interaction and recreation can promote well-being and foster a sense of community.
Addressing the Stigma Surrounding Mental Health in First Responder Communities
The culture of stoicism and self-reliance prevalent in many first responder communities often contributes to stigma surrounding mental health. Addressing this stigma requires a multifaceted approach involving education, open communication, and leadership commitment to prioritizing mental wellness.
Strategies for Reducing Stigma
Initiatives to reduce stigma should involve educational campaigns, peer support programs, and leadership actively promoting mental health awareness. Sharing personal stories of recovery can help destigmatize mental health issues and encourage help-seeking. Celebrating mental wellness as a strength, rather than a weakness, is crucial in shifting the culture.
Impact of a Culture of Stoicism
The traditional culture of stoicism and self-reliance within first responder communities can create a barrier to seeking help. This culture often discourages expressing vulnerability or admitting to struggles with mental health. Shifting this culture requires a concerted effort from leadership and the entire community.
Promoting Open Conversations About Mental Health
Open conversations about mental health can be fostered through educational workshops, peer support groups, and leadership actively engaging in discussions about mental well-being. Creating a safe and supportive environment where individuals feel comfortable sharing their experiences is crucial for breaking down stigma.
Long-Term Strategies for Sustaining Mental Wellness
Sustaining mental wellness among first responders requires ongoing commitment to preventative measures, access to resources, and the incorporation of self-care practices into daily life. A long-term strategy should incorporate a range of initiatives to promote resilience and well-being.
Ongoing Mental Health Support and Wellness Initiatives
Ongoing support should include regular mental health check-ups, access to therapy and peer support, and wellness programs focused on stress management, physical fitness, and healthy lifestyle choices. Regular training on stress management and coping skills can enhance resilience and prevent the development of mental health problems.
Importance of Preventative Measures and Access to Resources
Preventative measures are crucial in mitigating the risk of developing mental health issues. This includes proactive screening, access to mental health services, and educational programs promoting stress management and healthy coping mechanisms. Ensuring easy access to resources, such as EAPs and specialized mental health clinics, is essential.
Incorporating Regular Self-Care Practices
Self-care practices, such as regular exercise, healthy eating, sufficient sleep, and mindfulness techniques, are essential for maintaining mental well-being. Encouraging first responders to prioritize self-care and providing resources and support for these practices is vital for long-term mental health.
Future Directions and Research Needs in X-N Early Mental Health Intervention: X-n Early Mental Health Intervention For First Responders
Further research is needed to refine and improve early intervention strategies for first responders. This includes exploring innovative approaches, evaluating the effectiveness of existing programs, and fostering collaboration between researchers, healthcare professionals, and first responder organizations.
Areas Requiring Further Research
Further research is needed on the effectiveness of various intervention methods for different mental health conditions, the long-term impact of early interventions, and the role of specific risk factors in the development of mental health problems among first responders. Studies examining the effectiveness of culturally sensitive interventions are also crucial.
Potential Areas for Improvement in Existing Programs
Existing programs could be improved by enhancing accessibility, increasing cultural sensitivity, and incorporating technology to improve access to care. Improving collaboration between healthcare providers and first responder organizations is also essential for seamless care coordination.
Collaboration Between Researchers, Healthcare Professionals, and First Responder Organizations
Effective collaboration is essential for developing and implementing evidence-based interventions. This involves sharing data, coordinating research efforts, and ensuring that research findings are translated into practical strategies that can be implemented within first responder organizations. A collaborative approach is vital for creating sustainable change.
Ultimately, supporting the mental health of first responders requires a multifaceted approach. From implementing early intervention screening processes and providing access to various therapies and support programs, to fostering a culture of open communication and reducing stigma, we must prioritize their well-being. By working collaboratively – involving leadership, organizations, families, and communities – we can create a sustainable system of care that ensures these heroes receive the support they deserve, both during and after their service.
Share this content:
