You Have To Be Suicidal To Get Mental Healthcare
You have to be suicidal to get mental health care – a disheartening statement reflecting a grim reality for many. This misconception fuels the stigma surrounding mental illness, preventing countless individuals from seeking the help they desperately need. Limited access, high costs, and systemic barriers create a frustrating landscape where those struggling silently often find themselves further isolated and unable to navigate the complex system designed to support them.
This exploration delves into the root causes of this problem, highlighting the urgent need for reform and increased awareness.
The pervasive belief that only those on the brink of suicide can access mental healthcare is deeply damaging. It not only discourages early intervention but also reinforces the shame and fear that already prevent many from seeking help. This creates a vicious cycle where untreated mental health conditions worsen, leading to more severe consequences. This discussion will examine the systemic failures that contribute to this problem, explore solutions to improve access to care, and discuss the importance of preventative measures and public awareness campaigns.
The Frustrating Reality of Access to Mental Healthcare
Securing mental healthcare shouldn’t be a Herculean task, yet for many, it’s a frustrating and often insurmountable obstacle. Systemic barriers, financial constraints, and geographical limitations combine to create a system that fails to adequately serve those who need it most. This article explores these challenges and proposes solutions to improve access and reduce the pervasive stigma surrounding mental health.
Systemic Barriers to Mental Healthcare Access
Navigating the mental healthcare system often feels like navigating a maze. Complex referral processes, lengthy wait times for appointments, and a lack of coordination between different healthcare providers contribute to significant delays in receiving necessary treatment. This is further compounded by a shortage of mental health professionals, particularly in underserved communities, leading to long waitlists and limited availability of specialized services.
Financial Hurdles in Mental Healthcare, You have to be suicidal to get mental health care
The high cost of mental healthcare is a significant barrier for many individuals. Insurance coverage often falls short, leaving individuals with substantial out-of-pocket expenses for therapy sessions, medication, and hospitalization. Even with insurance, navigating deductibles, co-pays, and finding in-network providers can be a daunting process. This financial burden can force individuals to forgo necessary treatment, exacerbating their mental health challenges.
Geographical Limitations in Accessing Mental Healthcare
Access to mental healthcare is heavily influenced by geographical location. Rural and underserved areas often experience a severe shortage of mental health professionals, forcing individuals to travel long distances for appointments or rely on limited telehealth options which may not be suitable for everyone. This lack of accessibility disproportionately impacts individuals in these areas, leaving them with limited or no access to vital mental health services.
Bureaucratic Obstacles in Mental Healthcare
Bureaucratic hurdles further complicate access to mental healthcare. Complex authorization processes for treatments, lengthy paperwork requirements, and difficulties in navigating insurance claims create unnecessary delays and frustrations. These bureaucratic obstacles can be particularly challenging for individuals already struggling with their mental health, adding an extra layer of stress to an already difficult situation. Examples include needing multiple referrals before seeing a specialist or battling insurance companies to cover necessary treatments.
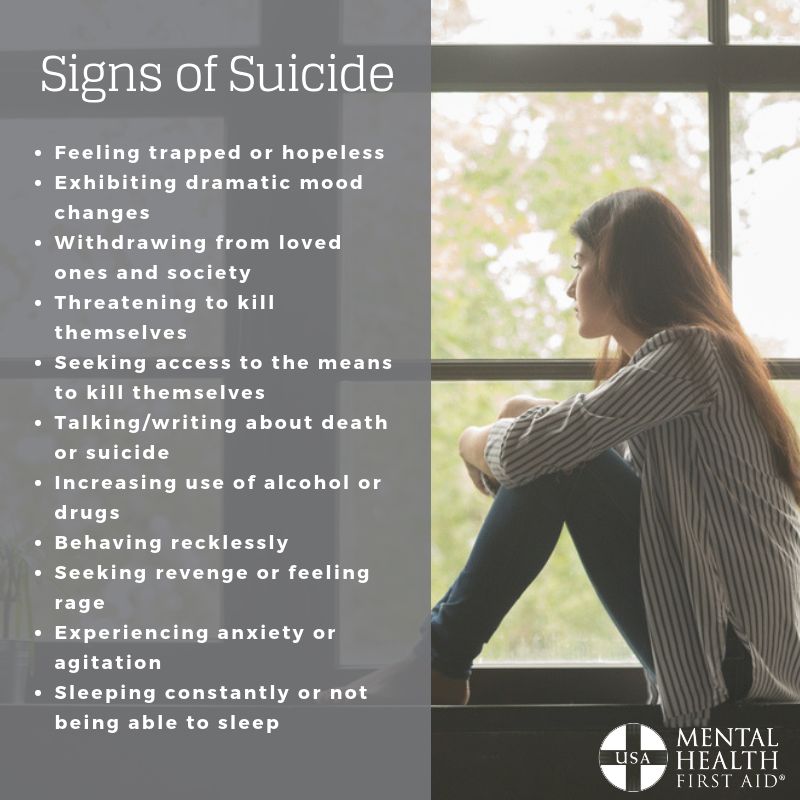
The Misconception: Suicidal Ideation as a Pre-requisite for Care
The harmful misconception that one must be suicidal to receive mental healthcare perpetuates stigma and prevents individuals from seeking help when they need it most. This belief is not only inaccurate but also incredibly dangerous, discouraging early intervention and potentially leading to severe consequences.
The Harmful Implications of the “Suicidal Ideation” Misconception
The statement “You have to be suicidal to get mental health care” is a dangerous oversimplification. It creates a false threshold for seeking help, implying that unless one is actively considering suicide, their mental health struggles are not serious enough to warrant professional attention. This misconception reinforces the stigma surrounding mental illness, making individuals hesitant to reach out for fear of judgment or dismissal.
Real-Life Examples of the Negative Impact of This Belief
Many individuals delay seeking help because they believe their symptoms are not severe enough to warrant professional intervention. They might feel ashamed or embarrassed to admit their struggles, fearing they will be labeled as “weak” or “crazy.” This delay can lead to worsening symptoms, impacting their relationships, work, and overall quality of life. For example, one individual postponed seeking help for anxiety for years, believing their concerns were trivial compared to those experiencing suicidal thoughts.
Their anxiety ultimately worsened, impacting their ability to maintain employment and social relationships.
A Public Awareness Campaign to Counteract the Misconception
A multi-pronged public awareness campaign is crucial to address this harmful misconception. The campaign should use various media platforms, including social media, television, and print advertisements, to disseminate accurate information about mental health and promote help-seeking behavior. The messaging should emphasize the importance of early intervention and preventative care, regardless of the severity of symptoms. The campaign should also feature testimonials from individuals who have successfully navigated the mental healthcare system, demonstrating that seeking help is a sign of strength, not weakness.
The Importance of Early Intervention and Preventative Care
Early intervention and preventative care are crucial for improving mental health outcomes. Addressing mental health concerns early can significantly reduce the severity and duration of challenges, preventing escalation to more serious conditions. Proactive measures can empower individuals to manage their mental well-being effectively.
Benefits of Early Intervention in Mental Health
Early intervention can significantly improve the prognosis for individuals experiencing mental health challenges. By addressing concerns early, professionals can help individuals develop coping mechanisms, manage symptoms, and prevent the development of more severe conditions. Early intervention can also help prevent disruptions to education, employment, and social relationships. This can lead to better long-term outcomes, improved quality of life, and reduced healthcare costs in the long run.
Preventative Care and Reducing the Severity of Mental Health Challenges
Preventative care focuses on promoting mental wellness and preventing the onset of mental health disorders. This involves teaching individuals healthy coping strategies, stress management techniques, and promoting a healthy lifestyle. By addressing risk factors early, preventative care can significantly reduce the likelihood of developing mental health problems or lessen the severity of existing conditions.
Resources and Strategies for Proactive Mental Wellness

Numerous resources are available to promote proactive mental wellness. These include mindfulness practices, regular exercise, a balanced diet, sufficient sleep, and strong social support networks. Seeking professional guidance from therapists or counselors can provide individuals with personalized strategies for managing stress, improving coping skills, and building resilience. Access to mental health apps and online resources can also be beneficial for individuals seeking support and information.
Preventative Measures for Improved Mental Well-being
- Regular exercise
- Mindfulness and meditation
- Healthy diet and sufficient sleep
- Strong social connections and support networks
- Stress management techniques
- Engaging in hobbies and activities that bring joy
- Seeking professional help when needed
Improving Access and Reducing Stigma
Improving access to mental healthcare requires a multi-faceted approach that addresses systemic barriers, financial constraints, and the pervasive stigma surrounding mental illness. Policy changes, community-based programs, and provider training are all essential components of creating a more equitable and supportive system.
Policy Changes to Improve Mental Healthcare Access
Policy changes are crucial to improving access to mental healthcare. These include increasing funding for mental health services, expanding insurance coverage to include a wider range of mental health treatments, and reducing bureaucratic barriers to care. Investing in telehealth infrastructure can improve access for individuals in rural and underserved areas. Additionally, implementing policies that prioritize early intervention and preventative care can help reduce the burden on the healthcare system in the long term.
Successful Community-Based Programs Addressing Mental Health Needs
Many successful community-based programs demonstrate the effectiveness of localized approaches to mental healthcare. These programs often focus on providing accessible and culturally sensitive services, building strong community partnerships, and reducing stigma through education and awareness campaigns. Examples include peer support groups, community mental health centers, and school-based mental health programs.
Practical Steps for Healthcare Providers to Reduce Stigma and Improve Patient Care
Healthcare providers play a vital role in reducing stigma and improving patient care. This involves providing empathetic and non-judgmental care, engaging in ongoing training on mental health issues, and actively challenging stigmatizing attitudes and beliefs within their own practices. Implementing trauma-informed care practices and utilizing person-centered approaches can significantly improve the patient experience and promote positive outcomes.
- Provide comprehensive and culturally sensitive training for all healthcare staff.
- Implement trauma-informed care practices.
- Use person-centered approaches to care.
- Actively challenge stigmatizing attitudes and beliefs.
- Advocate for policy changes that improve access to care.
Economic Benefits of Investing in Accessible Mental Healthcare
Investing in accessible and comprehensive mental healthcare offers significant economic benefits. Early intervention and preventative care can reduce healthcare costs in the long run by preventing the escalation of mental health challenges. Improved mental health also leads to increased productivity, reduced absenteeism, and lower rates of incarceration. A healthy population contributes to a stronger economy and a more vibrant society.
The Role of Public Awareness Campaigns: You Have To Be Suicidal To Get Mental Health Care
Comprehensive public awareness campaigns are essential to address the misconception that one must be suicidal to access mental healthcare. These campaigns should use multiple channels to reach a wide audience and effectively communicate the importance of mental health and seeking help.
Designing a Comprehensive Public Awareness Campaign
A successful campaign needs clear, concise messaging, relatable stories, and diverse representation. It should emphasize the normalcy of experiencing mental health challenges and the availability of support. The campaign should actively challenge the stigma surrounding mental illness and promote help-seeking behavior as a sign of strength, not weakness. Use of positive imagery and language is crucial to counter negative stereotypes.
Strategies for Effectively Communicating the Importance of Mental Health
Effective communication involves using diverse media platforms to reach different audiences. Social media campaigns can engage younger demographics, while television and radio ads can reach a broader audience. Partnerships with community organizations and influencers can help amplify the message and build trust. Using relatable stories and testimonials can humanize the issue and make it more accessible to the public.
Target Audiences and Tailored Messaging
Tailoring messages to specific target audiences is crucial for effective communication. For example, campaigns targeting young adults might emphasize peer support and online resources, while campaigns targeting older adults might focus on community-based programs and accessible healthcare services. Messages should be culturally sensitive and consider the unique needs and experiences of diverse populations.
Utilizing Different Media Platforms
A multi-platform approach is essential to reach a wide audience. Social media platforms like Instagram, TikTok, and Facebook allow for targeted advertising and interactive engagement. Television and radio ads provide broader reach, while print media can offer in-depth information and resources. Utilizing a variety of media channels ensures that the campaign’s message reaches diverse populations effectively.
The Impact on Individuals and Communities
Delayed or inaccessible mental healthcare has profound and long-lasting consequences for individuals and communities. Untreated mental illness can lead to significant personal hardship, decreased productivity, and increased societal costs. Addressing these challenges requires a comprehensive approach that considers the unique needs of diverse populations.
Long-Term Consequences of Delayed or Inaccessible Mental Healthcare
Delayed or inaccessible mental healthcare can have devastating consequences for individuals. Untreated mental illness can lead to chronic conditions, relationship problems, job loss, and increased risk of self-harm or suicide. It can also significantly impact an individual’s overall quality of life, limiting their ability to participate fully in society.
Societal Impact of Untreated Mental Illness
Untreated mental illness has significant societal costs. It impacts productivity, leading to lost workdays and reduced economic output. It can also increase healthcare costs, as untreated conditions often escalate to more severe stages requiring more intensive and expensive treatment. Furthermore, untreated mental illness can contribute to increased crime rates and social unrest.
Comparison of Mental Health Systems in Different Countries
Different countries have varying approaches to mental healthcare, with some demonstrating better outcomes than others. Countries with comprehensive universal healthcare systems often have better access to mental health services and lower rates of untreated mental illness. These systems prioritize early intervention, preventative care, and integration of mental health services into primary care. Studying successful models from other countries can inform the development of improved systems elsewhere.
Challenges Faced by Marginalized Communities in Accessing Mental Health Services
Marginalized communities, including racial and ethnic minorities, LGBTQ+ individuals, and people with disabilities, often face significant barriers in accessing mental health services. These barriers include cultural stigma, language barriers, discrimination, and lack of culturally competent providers. Addressing these inequities requires culturally sensitive services, language access programs, and provider training on cultural competency.
Ultimately, dismantling the misconception that one must be suicidal to receive mental healthcare requires a multifaceted approach. This includes addressing systemic barriers to access, increasing funding for mental health services, and launching comprehensive public awareness campaigns to reduce stigma and encourage early intervention. By promoting a culture of proactive mental wellness and providing readily available support, we can create a system that prioritizes the mental health of all individuals, not just those in crisis.
The journey to better mental healthcare is a collective responsibility, demanding action from individuals, communities, and policymakers alike.
Share this content:

