Medical billing and coding is the backbone of healthcare finance, ensuring providers get paid for the services they deliver. This intricate system translates complex medical procedures and diagnoses into standardized codes, which are then used to submit claims to insurance companies for reimbursement.
These professionals play a crucial role in keeping the healthcare system running smoothly, acting as the bridge between patient care and financial stability.
From understanding the various coding systems like ICD-10-CM and CPT to navigating the complexities of reimbursement methods and compliance regulations, this guide delves into the world of medical billing and coding, shedding light on its significance and the challenges it presents.
Introduction to Medical Billing and Coding
Medical billing and coding are essential components of the healthcare system, ensuring accurate financial transactions between patients, healthcare providers, and insurance companies. This field involves the translation of medical services and procedures into standardized codes, which are used to create invoices and process claims for reimbursement.
The Significance of Medical Billing and Coding
Medical billing and coding play a crucial role in maintaining the financial stability of healthcare providers. Accurate coding ensures that providers receive appropriate reimbursement for the services they deliver, enabling them to continue providing quality care. Additionally, it facilitates the collection and analysis of healthcare data, which is vital for research, public health initiatives, and improving patient outcomes.
The Role of Medical Billing and Coding Professionals
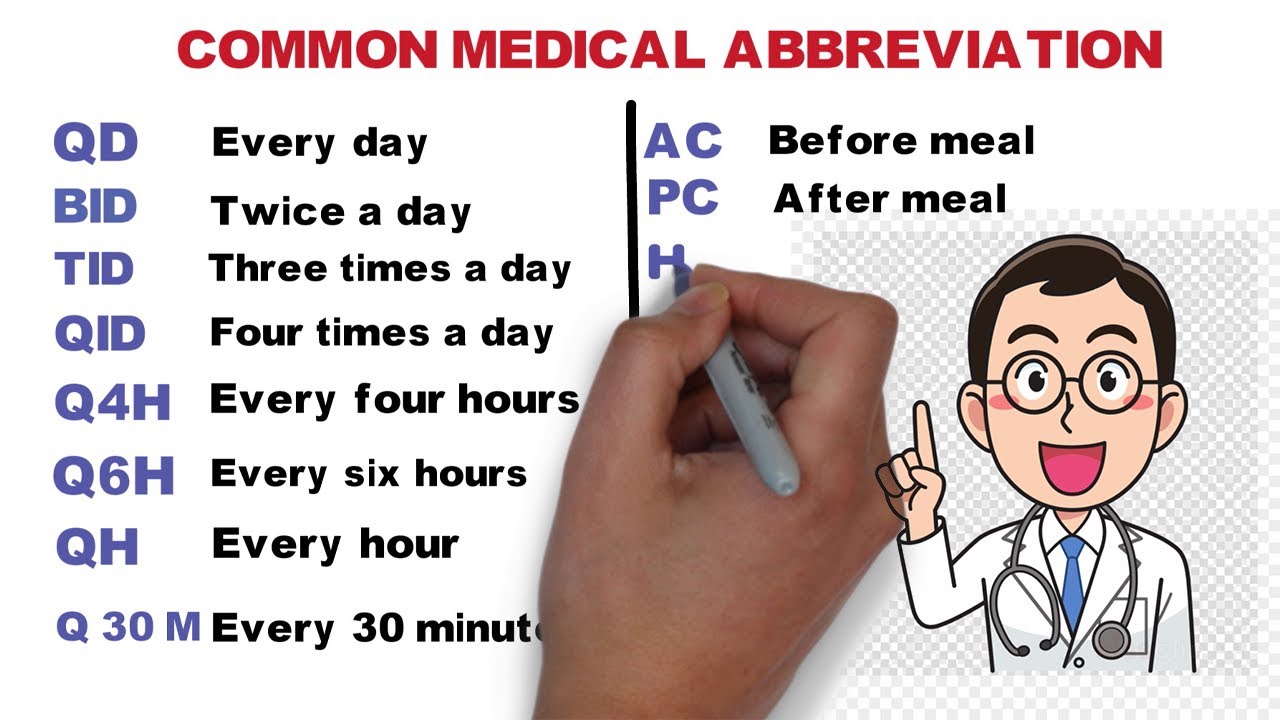
Medical billing and coding professionals are responsible for translating medical documentation into standardized codes, creating invoices, and processing claims for reimbursement. They work closely with physicians, nurses, and other healthcare professionals to ensure accurate and timely billing. Their expertise in medical terminology, coding systems, and billing regulations is essential for the smooth operation of healthcare facilities.
A Brief History of Medical Billing and Coding
The evolution of medical billing and coding can be traced back to the early 20th century, when the American Medical Association (AMA) introduced the first standardized coding system. Over time, the coding systems have evolved and become increasingly complex, reflecting the advancements in medical technology and healthcare practices.
The development of electronic health records (EHRs) has significantly impacted the field, automating many billing processes and facilitating data exchange.
The Medical Billing Process
The medical billing process involves a series of steps that ensure accurate and timely reimbursement for healthcare services. These steps include:
- Patient Registration and Demographics
- Medical Documentation and Chart Review
- Coding and Charge Entry
- Claims Submission and Processing
- Payment and Reconciliation
- Denial Management and Appeals
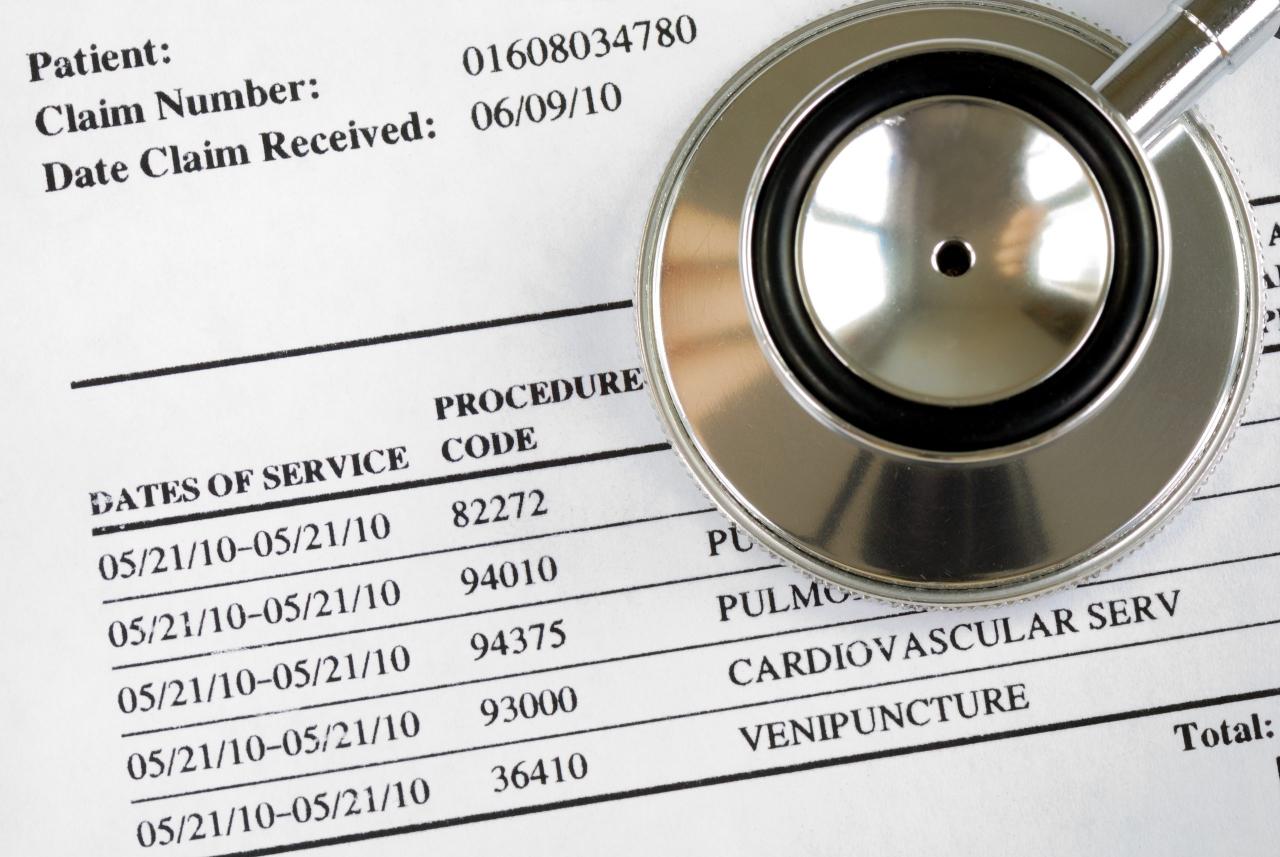
Examples of Medical Billing Codes
Medical billing codes are used to represent specific medical services, procedures, and diagnoses. Some common types of codes include:
- CPT Codes (Current Procedural Terminology):These codes represent medical procedures and services performed by physicians and other healthcare professionals.
- ICD-10-CM Codes (International Classification of Diseases, Tenth Revision, Clinical Modification):These codes represent diagnoses, symptoms, and medical conditions.
- HCPCS Codes (Healthcare Common Procedure Coding System):These codes are used for medical services, supplies, and procedures not covered by CPT codes.
The Role of Electronic Health Records (EHRs) in Medical Billing
EHRs have revolutionized medical billing by automating many processes and improving data accuracy. They facilitate the capture and storage of patient information, streamline coding and charge entry, and enable seamless claims submission. EHRs also enhance communication between providers and insurance companies, reducing the risk of billing errors and delays.
Medical Coding Systems
Medical coding systems are standardized classifications used to represent medical services, procedures, and diagnoses. These systems are essential for accurate billing, claims processing, and data analysis in healthcare.
Major Medical Coding Systems in the United States
The two primary medical coding systems used in the United States are:
- ICD-10-CM (International Classification of Diseases, Tenth Revision, Clinical Modification):This system is used to classify diagnoses, symptoms, and medical conditions. It contains over 14,000 codes, each representing a specific medical condition or diagnosis.
- CPT (Current Procedural Terminology):This system is used to classify medical procedures and services performed by physicians and other healthcare professionals. It includes over 10,000 codes, each representing a specific medical procedure or service.
Comparison of ICD-10-CM and CPT Codes
| Feature | ICD-10-CM | CPT |
|---|---|---|
| Purpose | Classifying diagnoses and medical conditions | Classifying medical procedures and services |
| Code Structure | Alphanumeric, with a maximum of 7 characters | Numeric, with a maximum of 5 digits |
| Specificity | Highly specific, with codes for various levels of detail | More focused on procedures and services, with less emphasis on specific conditions |
| Use | Used for billing, claims processing, and data analysis | Used for billing, claims processing, and physician documentation |
Structure of a Medical Code
Medical codes typically follow a specific structure, with each digit or character representing a specific element of the code. For example, an ICD-10-CM code might be structured as follows:
Chapter
- Subchapter
- Category
- Subcategory
- Code
This structure allows for clear and concise communication of medical information between healthcare providers, insurance companies, and other stakeholders.
Reimbursement and Payment Methods
Reimbursement in healthcare refers to the payment received by providers for the services they deliver. Different payment methods are used in the healthcare system, each with its own rules and regulations.
Different Payment Methods in Healthcare
- Fee-for-Service:This traditional method involves paying providers a set fee for each service rendered. It is often based on a fee schedule established by the insurance company or government agency.
- Managed Care:This method involves contracting with healthcare providers to deliver services to a specific group of patients at a predetermined rate. It emphasizes cost containment and preventive care.
- Value-Based Care:This model focuses on rewarding providers for the quality of care they deliver, rather than the quantity of services provided. It encourages providers to improve patient outcomes and reduce costs.
Healthcare Claims Processing
Claims processing involves the review and evaluation of healthcare claims submitted by providers to insurance companies. Insurance companies use a set of criteria to determine the appropriateness and necessity of the services billed, and to calculate the amount of reimbursement due to the provider.
The claims processing system ensures that providers are paid fairly for the services they deliver.
The Role of Insurance Companies in Medical Billing
Insurance companies play a critical role in medical billing by acting as intermediaries between patients and providers. They provide financial protection to patients, covering a portion of the costs associated with healthcare services. Insurance companies also establish payment policies and fee schedules, which guide the reimbursement process.
Compliance and Regulations
Medical billing is subject to a complex legal and regulatory framework designed to ensure accuracy, transparency, and compliance with healthcare laws. These regulations govern various aspects of billing, including coding, claim submission, and reimbursement.
Legal and Regulatory Framework Governing Medical Billing
- HIPAA (Health Insurance Portability and Accountability Act):This federal law protects patient privacy and ensures the secure handling of protected health information (PHI).
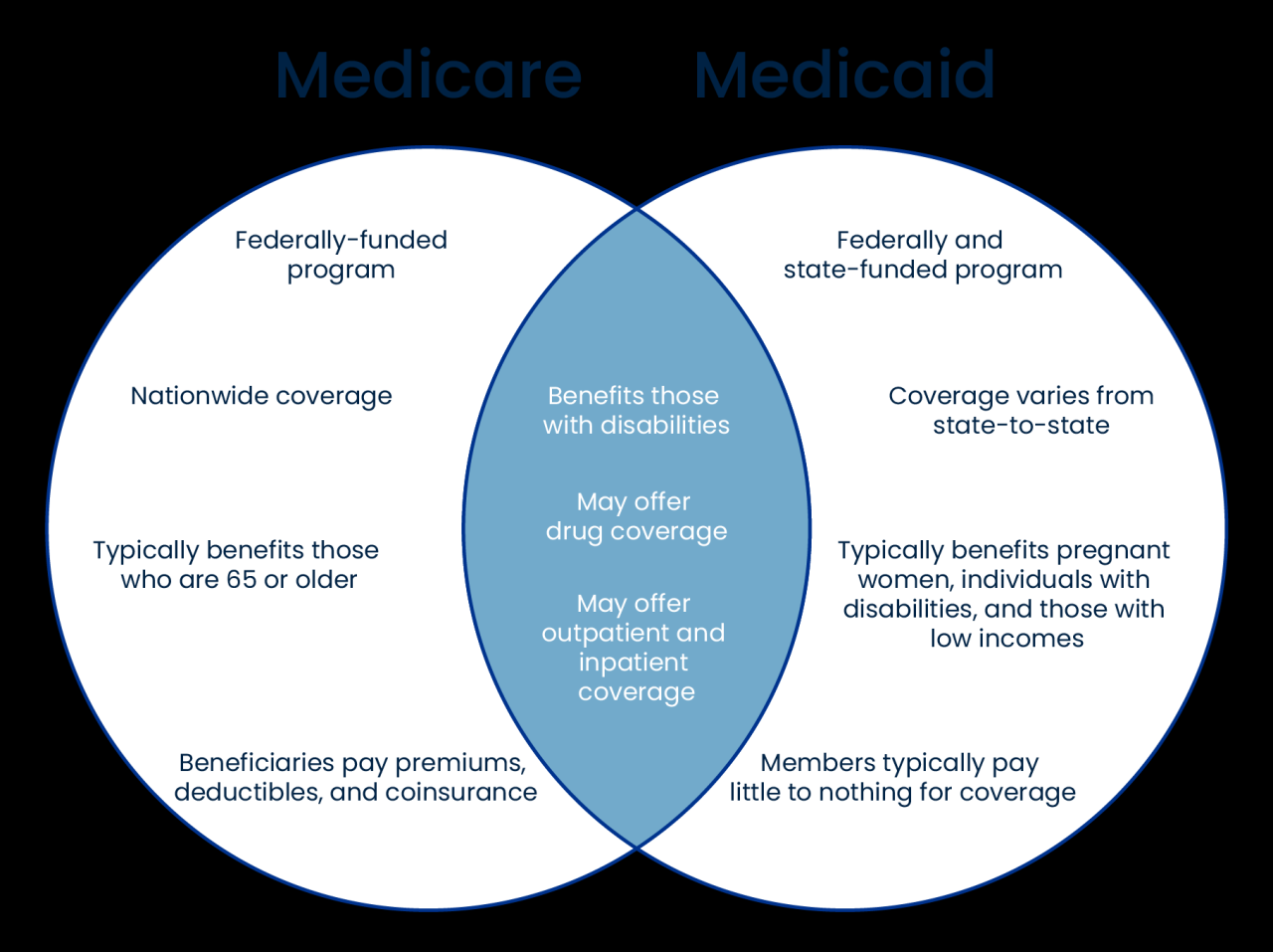
- Medicare and Medicaid:These federal programs have specific rules and regulations governing billing and reimbursement for services provided to Medicare and Medicaid beneficiaries.
- State Laws:Each state has its own regulations regarding medical billing, including requirements for licensing and credentialing.
Common Billing Errors and Their Consequences
Billing errors can have significant consequences for providers, including:
- Delayed or Denied Claims:Inaccurate coding or incomplete documentation can lead to claims being rejected or delayed, impacting cash flow and revenue.
- Audits and Investigations:Billing errors can trigger audits and investigations by insurance companies or government agencies, potentially leading to fines or penalties.
- Reputational Damage:Repeated billing errors can damage a provider’s reputation and erode patient trust.
Resources for Staying Up-to-Date on Billing Regulations
Staying informed about the latest billing regulations is crucial for compliance and avoiding errors. Some helpful resources include:
- Centers for Medicare & Medicaid Services (CMS):The CMS website provides information on Medicare and Medicaid billing regulations.
- American Health Information Management Association (AHIMA):AHIMA offers resources, education, and certification programs for medical billing and coding professionals.
- American Medical Association (AMA):The AMA publishes the CPT coding manual and provides resources on billing and coding best practices.
The Future of Medical Billing and Coding
The field of medical billing and coding is constantly evolving, driven by technological advancements, changing healthcare models, and increasing regulatory scrutiny. These factors will continue to shape the future of the profession, presenting both challenges and opportunities for professionals.
Impact of Technology on Medical Billing and Coding
Technology is playing an increasingly significant role in medical billing and coding, automating many processes and improving efficiency. Artificial intelligence (AI) and machine learning are being used to streamline coding, detect errors, and enhance claims processing. Cloud-based platforms and mobile applications are also transforming the way billing professionals work, providing access to information and tools from anywhere at any time.
Emerging Trends in Medical Billing and Coding
- Telehealth:The rise of telehealth is creating new billing challenges and opportunities. Providers need to ensure accurate coding for virtual visits and remote patient monitoring services.
- Value-Based Care:The shift toward value-based care models is emphasizing the importance of quality reporting and performance metrics in billing. Providers need to track and report outcomes to demonstrate the value of their services.
- Interoperability:The growing focus on interoperability is driving the need for standardized data exchange between healthcare providers and insurance companies. This will streamline billing processes and improve data accuracy.
Timeline of Potential Future Developments
The future of medical billing and coding is likely to be characterized by continued technological advancements, evolving payment models, and increasing regulatory complexity. Here is a timeline outlining some potential future developments:
- Short Term (1-3 Years):Widespread adoption of AI and machine learning for coding and claims processing, increased use of cloud-based billing platforms, and further development of telehealth billing guidelines.
- Medium Term (3-5 Years):Expansion of value-based care models, requiring more sophisticated data analytics and performance reporting. Increased focus on interoperability and data exchange between healthcare systems.
- Long Term (5+ Years):Development of new coding systems and payment models to reflect advancements in medical technology and healthcare practices. Potential for blockchain technology to improve security and transparency in medical billing.
Closing Summary
The future of medical billing and coding is poised for transformation, driven by the integration of technology and evolving healthcare trends. As healthcare continues to embrace electronic health records (EHRs), telehealth, and value-based care models, medical billing and coding professionals must adapt to stay ahead of the curve.
By embracing new technologies and staying informed about the latest regulations, these professionals can ensure the continued success of the healthcare industry.