Migraine medication sets the stage for this exploration, offering a deep dive into the various approaches to managing this debilitating condition. Whether you’re seeking relief from an acute attack or looking for long-term prevention strategies, understanding the options available is crucial.
This guide will illuminate the different classes of medications, their mechanisms of action, and potential side effects, helping you navigate the world of migraine treatment.
From triptans to non-triptan medications and preventive therapies, we’ll delve into the intricacies of each approach. We’ll also explore the importance of lifestyle modifications and the potential for drug interactions. This comprehensive overview aims to equip you with the knowledge you need to make informed decisions about your migraine management.
Migraine Medication Overview
Migraines are a common and often debilitating type of headache that can significantly impact a person’s quality of life. The good news is that there are various medications available to treat migraines, offering relief from the intense pain and associated symptoms.
This article provides a comprehensive overview of migraine medication, exploring different types, mechanisms of action, potential side effects, and important considerations for safe and effective use.
Types of Migraine Medications
Migraine medications can be broadly categorized into two main groups: acute medications used to treat migraine attacks as they occur, and preventive medications used to reduce the frequency and severity of migraines.
Acute Migraine Medications
Acute migraine medications are designed to stop a migraine attack once it has started. They work by targeting specific pathways in the brain that are involved in migraine pain and inflammation.
Triptans
Triptans are a class of medications that are highly effective in treating acute migraine attacks. They work by constricting blood vessels in the brain and blocking the release of inflammatory substances.
- Sumatriptan (Imitrex)
- Zolmitriptan (Zomig)
- Rizatriptan (Maxalt)
- Naratriptan (Amerge)
- Almotriptan (Axert)
- Frovatriptan (Frova)
Non-Triptan Medications
Non-triptan medications offer alternative options for migraine relief. They work through different mechanisms, such as blocking pain signals, reducing inflammation, or calming the stomach.
- NSAIDs (Nonsteroidal Anti-inflammatory Drugs): Ibuprofen (Advil, Motrin), Naproxen (Aleve), Diclofenac (Voltaren)
- Antiemetics: Prochlorperazine (Compazine), Metoclopramide (Reglan)
- Ergot Alkaloids: Dihydroergotamine (DHE 45), Ergotamine (Cafergot)
Preventive Migraine Medications
Preventive migraine medications are taken daily to reduce the frequency and severity of migraine attacks. They work by targeting different pathways involved in migraine development, such as neurotransmitter imbalances or inflammation.
- Beta-blockers: Propranolol (Inderal), Metoprolol (Lopressor), Atenolol (Tenormin)
- Anticonvulsants: Topiramate (Topamax), Valproic acid (Depakote), Gabapentin (Neurontin)
- Antidepressants: Amitriptyline (Elavil), Venlafaxine (Effexor), Nortriptyline (Pamelor)
Triptans for Migraine Relief

Triptans are a mainstay of acute migraine treatment, offering rapid and effective relief for many individuals. They work by targeting serotonin receptors in the brain, constricting blood vessels, and reducing inflammation.
Effectiveness of Triptans
Triptans are generally considered highly effective in treating acute migraine attacks. Studies have shown that triptans can provide significant pain relief within 2 hours of administration, with many patients experiencing complete resolution of their symptoms.
If you’re interested in a career in healthcare, becoming a medical assistant could be a great option. They play a vital role in medical offices, assisting doctors and nurses with various tasks like taking patient histories, scheduling appointments, and drawing blood.
It’s a fast-growing field with a lot of opportunities for those who enjoy working directly with patients.
Comparing Triptans
Different triptans have varying onset of action, duration of effect, and potential side effects. Choosing the right triptan for an individual depends on their specific needs and preferences.
| Triptan | Dosage | Route of Administration | Onset of Action | Duration of Action | Common Side Effects |
|---|---|---|---|---|---|
| Sumatriptan (Imitrex) | 25-100 mg | Oral, nasal spray, subcutaneous injection | 30-60 minutes | 2-4 hours | Dizziness, drowsiness, tingling sensations |
| Zolmitriptan (Zomig) | 2.5-5 mg | Oral, nasal spray | 30-60 minutes | 4-8 hours | Dizziness, fatigue, nausea |
| Rizatriptan (Maxalt) | 10 mg | Oral | 30-60 minutes | 4-6 hours | Dizziness, fatigue, drowsiness |
| Naratriptan (Amerge) | 2.5 mg | Oral | 1-2 hours | 12-24 hours | Dizziness, fatigue, dry mouth |
| Almotriptan (Axert) | 12.5 mg | Oral | 30-60 minutes | 6-8 hours | Dizziness, drowsiness, nausea |
| Frovatriptan (Frova) | 2.5 mg | Oral | 1-2 hours | 24 hours | Dizziness, fatigue, drowsiness |
Triptans for Specific Conditions
Certain triptans may be more suitable for individuals with specific medical conditions or contraindications. For example, individuals with cardiovascular disease may need to avoid certain triptans due to their potential to constrict blood vessels.
Non-Triptan Medications for Migraine
Non-triptan medications offer a range of options for migraine management, addressing different aspects of the migraine experience. They work through mechanisms distinct from triptans, providing alternative approaches to pain relief and symptom management.
Mechanisms of Action
Non-triptan medications for migraine relief work through various mechanisms, including:
- NSAIDs (Nonsteroidal Anti-inflammatory Drugs): Reduce inflammation and pain by inhibiting the production of prostaglandins.
- Antiemetics: Block signals in the brain that trigger nausea and vomiting, often associated with migraine attacks.
- Ergot Alkaloids: Constrict blood vessels in the brain, similar to triptans, but with a longer duration of action.
Examples of Non-Triptan Medications
Commonly used non-triptan medications for migraine relief include:
- Ibuprofen (Advil, Motrin): A widely available NSAID that provides pain relief and reduces inflammation.
- Naproxen (Aleve): Another NSAID with a longer duration of action than ibuprofen.
- Prochlorperazine (Compazine): An antiemetic that helps control nausea and vomiting associated with migraine attacks.
- Metoclopramide (Reglan): An antiemetic that also speeds up gastric emptying, which can be helpful for migraine-related nausea.
- Dihydroergotamine (DHE 45): An ergot alkaloid that provides long-lasting relief from migraine pain.
Benefits and Limitations
Non-triptan medications can offer significant benefits for migraine management, providing relief from pain, nausea, and other symptoms. However, they may not be as effective as triptans for all individuals, and some may have side effects or contraindications.
Preventive Migraine Medications
Preventive migraine medications are taken daily to reduce the frequency and severity of migraine attacks. They are not intended to stop a migraine attack once it has started, but rather to prevent them from occurring in the first place.
Purpose of Preventive Medications
Preventive migraine medications are often used for individuals who experience frequent or severe migraines that significantly impact their daily lives. They aim to reduce the number of migraine days per month and improve overall quality of life.
Classes of Preventive Medications
Preventive migraine medications belong to different classes, each with its own mechanism of action and potential side effects.
- Beta-blockers: These medications block the action of adrenaline, a hormone that can trigger migraines in some individuals.
- Anticonvulsants: These medications are typically used to treat seizures, but they can also be effective in preventing migraines by stabilizing brain activity.
- Antidepressants: Some antidepressants, particularly tricyclic antidepressants, can help prevent migraines by regulating neurotransmitter levels in the brain.
Examples of Preventive Medications
Commonly prescribed preventive migraine medications include:
- Propranolol (Inderal): A beta-blocker that is often used to prevent migraines, especially in individuals with high blood pressure.
- Topiramate (Topamax): An anticonvulsant that can be effective in preventing migraines and may also help with weight loss.
- Amitriptyline (Elavil): A tricyclic antidepressant that can be effective in preventing migraines, but it can cause drowsiness and other side effects.
Side Effects and Long-Term Considerations
Preventive migraine medications can have side effects, and some may require long-term use. It’s important to discuss the potential risks and benefits with a healthcare professional to determine the best course of treatment.
Lifestyle Modifications for Migraine Management
Lifestyle modifications can play a significant role in migraine prevention and treatment. By identifying and managing triggers, individuals can reduce the frequency and severity of their migraines and improve their overall well-being.
Triggers of Migraines
Migraines are often triggered by specific factors, including:
- Stress: Emotional or physical stress can trigger migraine attacks in many individuals.
- Sleep Deprivation: Lack of sleep or inconsistent sleep patterns can increase the risk of migraines.
- Certain Foods: Some foods, such as aged cheeses, processed meats, and chocolate, can trigger migraines in susceptible individuals.
- Caffeine: Both caffeine withdrawal and excessive caffeine intake can trigger migraines.
- Alcohol: Alcohol consumption, particularly red wine, can trigger migraines in some individuals.
- Hormonal Changes: Fluctuations in hormone levels, such as those associated with menstruation or menopause, can trigger migraines.
- Weather Changes: Sudden changes in weather, such as barometric pressure shifts, can trigger migraines.
- Bright Lights: Exposure to bright lights, especially fluorescent lights, can trigger migraines in some individuals.
- Strong Odors: Certain strong odors, such as perfumes or smoke, can trigger migraines.
Managing Triggers
Strategies for managing migraine triggers include:
- Stress Management: Techniques such as yoga, meditation, or deep breathing exercises can help reduce stress levels.
- Regular Sleep Schedule: Aim for 7-8 hours of sleep per night and maintain a consistent sleep schedule.
- Food Diary: Keep track of foods consumed and note any potential triggers.
- Limit Caffeine and Alcohol: Moderate or avoid caffeine and alcohol consumption.
- Avoid Strong Odors: Minimize exposure to strong odors and perfumes.
- Wear Sunglasses: Protect eyes from bright light, especially during outdoor activities.
| Lifestyle Modification | Potential Benefits |
|---|---|
| Stress Management | Reduced frequency and severity of migraines |
| Regular Sleep Schedule | Improved sleep quality and reduced migraine risk |
| Food Diary | Identification and avoidance of food triggers |
| Limit Caffeine and Alcohol | Reduced migraine frequency and severity |
| Avoid Strong Odors | Reduced migraine triggers |
| Wear Sunglasses | Protection from bright light and reduced migraine risk |
Migraine Medication Safety and Interactions
Migraine medications, like any other medications, can have potential drug interactions and side effects. It’s crucial to use them safely and appropriately to minimize risks and maximize benefits.
Drug Interactions
Migraine medications can interact with other medications, including:
- Other migraine medications: Using multiple migraine medications at the same time can increase the risk of side effects.
- Antidepressants: Some antidepressants can interact with triptans, increasing the risk of serotonin syndrome.
- Antibiotics: Certain antibiotics can interfere with the effectiveness of triptans.
- Ergot alkaloids: Using triptans and ergot alkaloids together can increase the risk of cardiovascular problems.
Pregnancy and Breastfeeding
The safety of migraine medications during pregnancy and breastfeeding is a complex issue. It’s essential to discuss the risks and benefits with a healthcare professional before taking any migraine medication during these periods.
Medical Conditions
Individuals with specific medical conditions, such as cardiovascular disease, liver disease, or kidney disease, may need to avoid certain migraine medications or use them with caution.
Long-Term Use
Long-term use of migraine medications can increase the risk of side effects, such as dependence, tolerance, or withdrawal symptoms. It’s important to discuss the risks and benefits of long-term use with a healthcare professional.
Migraine Medication Research and Future Directions
Research in the field of migraine medication development is ongoing, with promising new therapies and treatment strategies emerging.
Emerging Therapies
New therapies under development for migraine include:
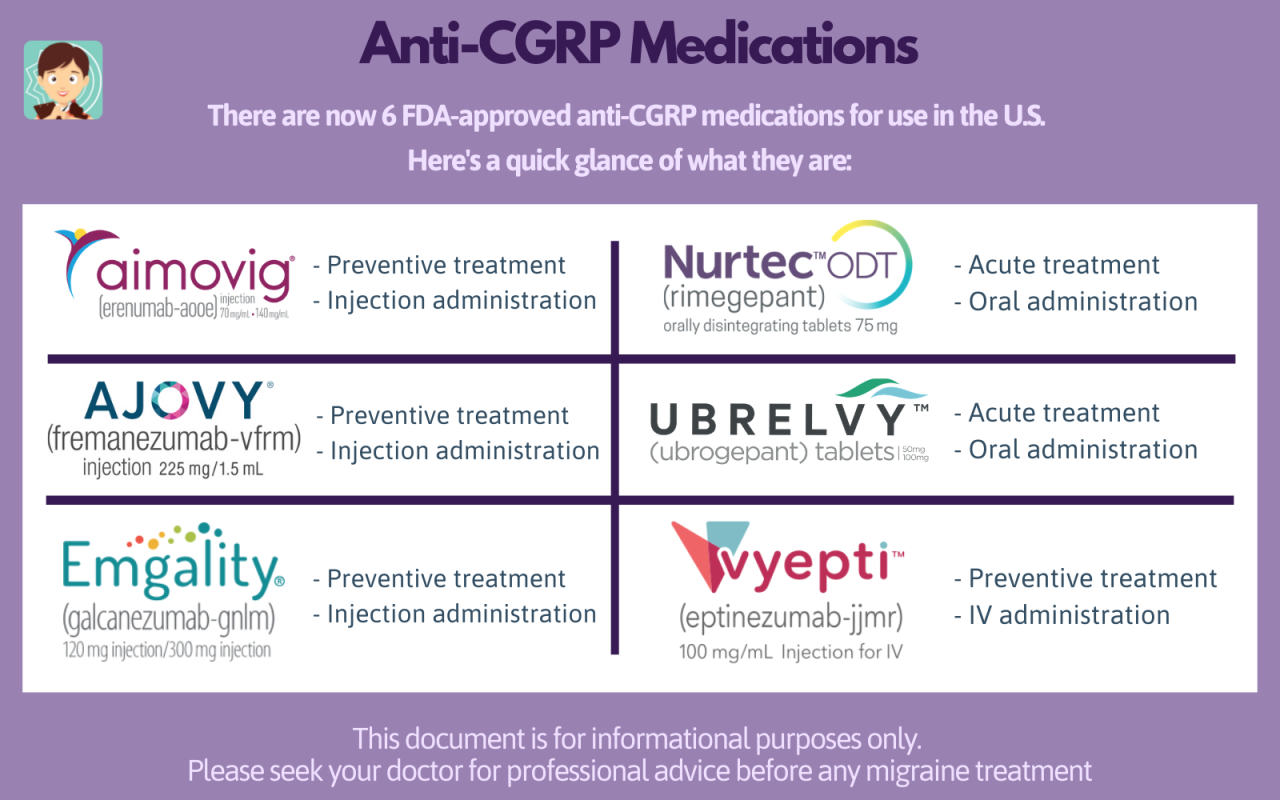
- CGRP (Calcitonin Gene-Related Peptide) Inhibitors: These medications block the action of CGRP, a neuropeptide that plays a role in migraine pain and inflammation.
- Monoclonal Antibodies: These medications target specific proteins involved in migraine development, offering long-term prevention.
- Neuromodulation Therapies: Techniques such as transcranial magnetic stimulation (TMS) and vagus nerve stimulation (VNS) aim to modulate brain activity and reduce migraine frequency.
Future of Migraine Medication
The future of migraine medication holds exciting possibilities, with ongoing research exploring new targets, delivery methods, and personalized treatment approaches.
If you’re interested in a career in healthcare but don’t want to be a doctor or nurse, becoming a medical assistant could be a great option. Medical assistants work closely with doctors and nurses, assisting with a wide range of tasks, from taking patient histories and vital signs to preparing exam rooms and administering medications.
Key Areas for Research
Further research is needed to:
- Develop more effective and targeted medications with fewer side effects.
- Improve our understanding of the underlying mechanisms of migraine.
- Develop personalized treatment plans tailored to individual needs and triggers.
- Explore alternative therapies, such as acupuncture, massage, and biofeedback.
Closure: Migraine Medication
Navigating the world of migraine medication can feel overwhelming, but armed with knowledge and understanding, you can find the path to relief. By carefully considering the various treatment options, their potential benefits and drawbacks, and your individual needs, you can work with your healthcare provider to create a personalized plan for managing your migraines.
Remember, you’re not alone, and there are resources available to help you on your journey to a life less burdened by migraine pain.